Cancer & Immunotherapy
Overview
Cancer is the second leading cause of death worldwide, after heart disease. However, the risk of dying from cancer has decreased over the past few decades due in part to advances in treatments, diagnosis and prevention — some that have notably been made at UCLA.
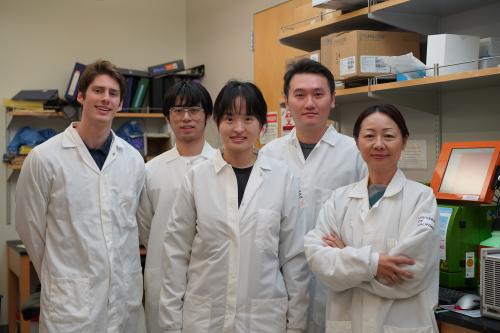
Partnering closely with the UCLA Health Jonsson Comprehensive Cancer Center, our researchers are developing novel stem-cell based therapies and bringing them to clinical trials to help patients battling some of the most aggressive, treatment-resistant cancers. As they work to better understand the characteristics of cancer — what makes cancer cells grow and spread — they’re uncovering new ways to exploit the weaknesses of these cells. These insights will lead to discoveries that could build on recent progress and dramatically shift the future of cancer treatment.
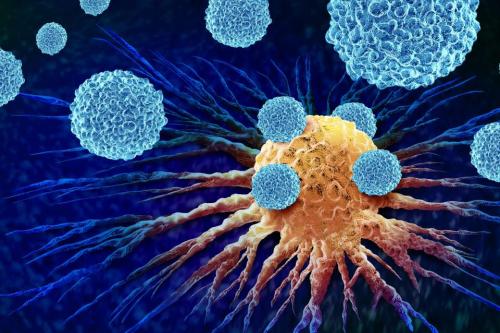
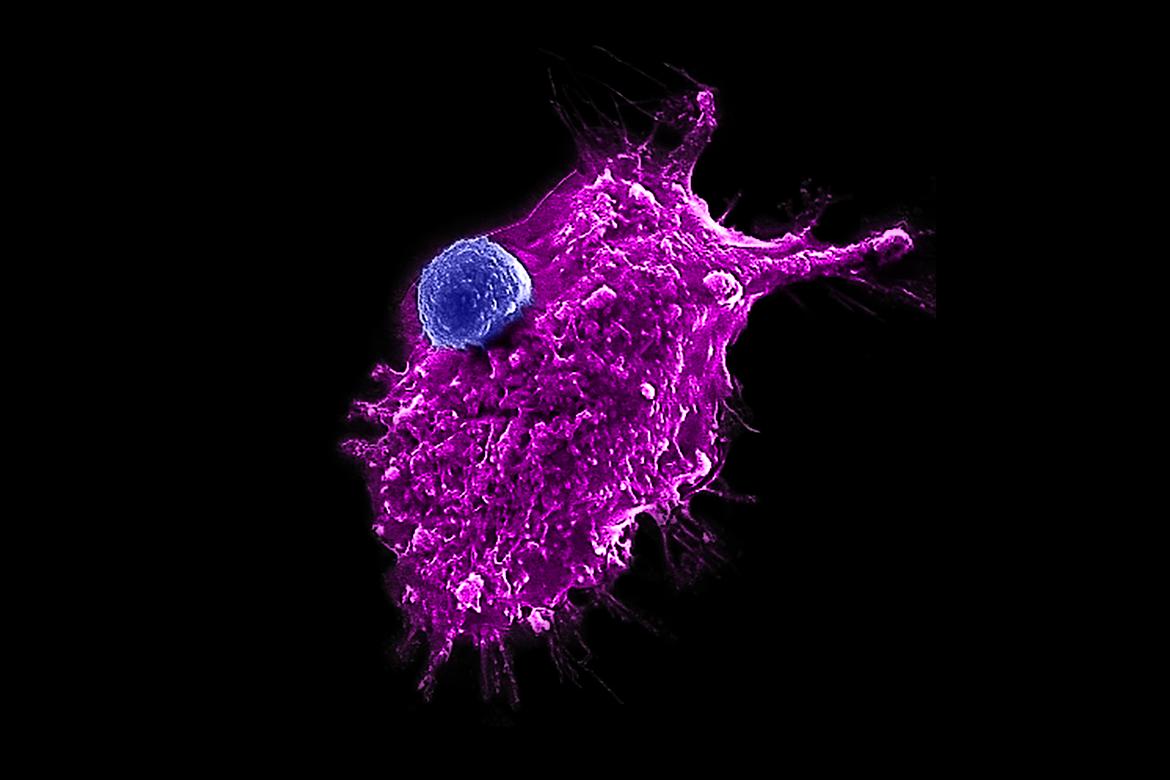
Several projects focus on optimizing currently available and future immunotherapy A type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions. immunotherapy A type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions. approaches by devising innovative strategies to make them more effective, safe and accessible. For example, our scientists are creating a gene-engineered platform that produces universal, off-the-shelf A type of "universal" cell therapy that can safely be used in any person. These experimental therapies rely on healthy donor cells that — either due to their unique properties or thanks to genetic modification — do not carry the risk of being rejected by patients' immune systems. Because these therapies do not have to be manufactured on a patient-specific basis, they can benefit more patients and reach them in a faster, more cost-effective way. off-the-shelf A type of "universal" cell therapy that can safely be used in any person. These experimental therapies rely on healthy donor cells that — either due to their unique properties or thanks to genetic modification — do not carry the risk of being rejected by patients' immune systems. Because these therapies do not have to be manufactured on a patient-specific basis, they can benefit more patients and reach them in a faster, more cost-effective way. CAR-T cells to make T-cell immunotherapy more widely available for the treatment of a range of cancers, including blood cancers like leukemia and multiple myeloma and solid organ cancers like brain, breast and prostate cancer. They’re also developing an injectable personalized cancer vaccine booster to treat and prevent tumor recurrence, a medical challenge current treatments such as chemotherapy and radiation can’t effectively address.
Our Goals
- Develop methods to produce large numbers of stem cell-derived cancer-fighting immune cells to pave the way for an "off-the-shelf" cancer immunotherapy A type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions. immunotherapy A type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions., which could be more affordable and accessible than currently available approaches
- Engineer smarter and stronger CAR-T cells to improve the safety and efficacy of therapies for patients with lymphoma, multiple myeloma and glioblastoma
- Develop novel mRNA Short for messenger ribonucleic acid, this single-stranded molecular plays a crucial role in protein synthesis within cells. Specifically, it carries the genetic information encoded in DNA to the ribosomes, where it is "read" to assemble proteins based on the code. mRNA Short for messenger ribonucleic acid, this single-stranded molecular plays a crucial role in protein synthesis within cells. Specifically, it carries the genetic information encoded in DNA to the ribosomes, where it is "read" to assemble proteins based on the code. cancer vaccines and therapeutics
- Develop new therapies that target the genomic instability of fast-growing and hard-to-treat cancers, including glioblastoma, melanoma and small cell neuroendocrine cancers
- Advance and clinically translate liquid biopsy diagnostic methods that leverage nanotechnologies to enable early detection of pediatric cancers
- Develop innovative treatments that empower senior patients to live longer, healthier lives by exploring the complex relationship between aging and cancer
- Develop T-cell receptor and CAR-T-based cellular immunotherapies that target multiple stages of prostate cancer as well as highly aggressive small cell carcinomas of the lung and other tissues
- Identify new and existing drugs and compounds that, when combined with immunotherapies, make these cancer treatments more effective
- Identify specific types of liver cancer stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves. stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves. that might be effectively targeted by natural killer cell-based immunotherapies
- Use computer modeling to understand how heat-based treatments affect the tumor microenvironment
Research Highlights
Defining metabolic flexibility in a skin cancer
UCLA scientists identify key metabolic mechanisms that squamous cell skin cancers use to resist treatment, offering new insights into how to potentially stop cancer growth.
Effective and affordable cell therapies
Our scientists develop a new method to engineer more powerful immune cells that could one day be used for “off-the-shelf” cell therapies for hard-to-treat cancers.
AI model predicts survival outcomes for cancer patients
UCLA researchers develop an AI model that successfully predicts patient outcomes across multiple cancer types by examining the gene expression patterns of epigenetic factors.
CAR-T cell immunotherapy shows promise
Center investigators develop a dual target CAR-T cell therapy for non-Hodgkin’s lymphoma that has successfully treated 10 of 11 patients in a Phase 1 clinical trial.
Novel treatment for advanced sarcomas
Center investigators launch a Phase 1 clinical trial of a stem cell immunotherapy for metastatic sarcoma.
Creating a renewable source of cancer-fighting T cells
Our researchers discover a technique that could produce an unlimited supply of T cells, a key step toward developing more widely accessible T cell therapies.
Collaborating to combat ovarian cancer
UCLA scientists are collaborating to develop a novel immunotherapy they hope will transform ovarian cancer treatment and reduce the likelihood of recurrence at a fraction of the cost of current therapies.
Immunotherapy for aggressive tumors
Center scientists develop an immunotherapy that shrinks or eliminates tumors in 90% of clinical trial participants with a rare and aggressive form of skin cancer.
Fighting cancer with SSRIs
UCLA scientists find that a widely used antidepressant drug could help the immune system fight cancer and suppress tumor growth.