Cristina Puig-Saus, Ph.D.
- Assistant Professor, Microbiology, Immunology and Molecular Genetics
- Assistant Professor, Surgical Oncology

Cristina Puig-Saus, Ph.D., specializes in developing novel cancer immunotherapies. Her work focuses on understanding natural T-cell responses to cancer, as well as designing and clinically translating new cellular therapies for solid tumors.
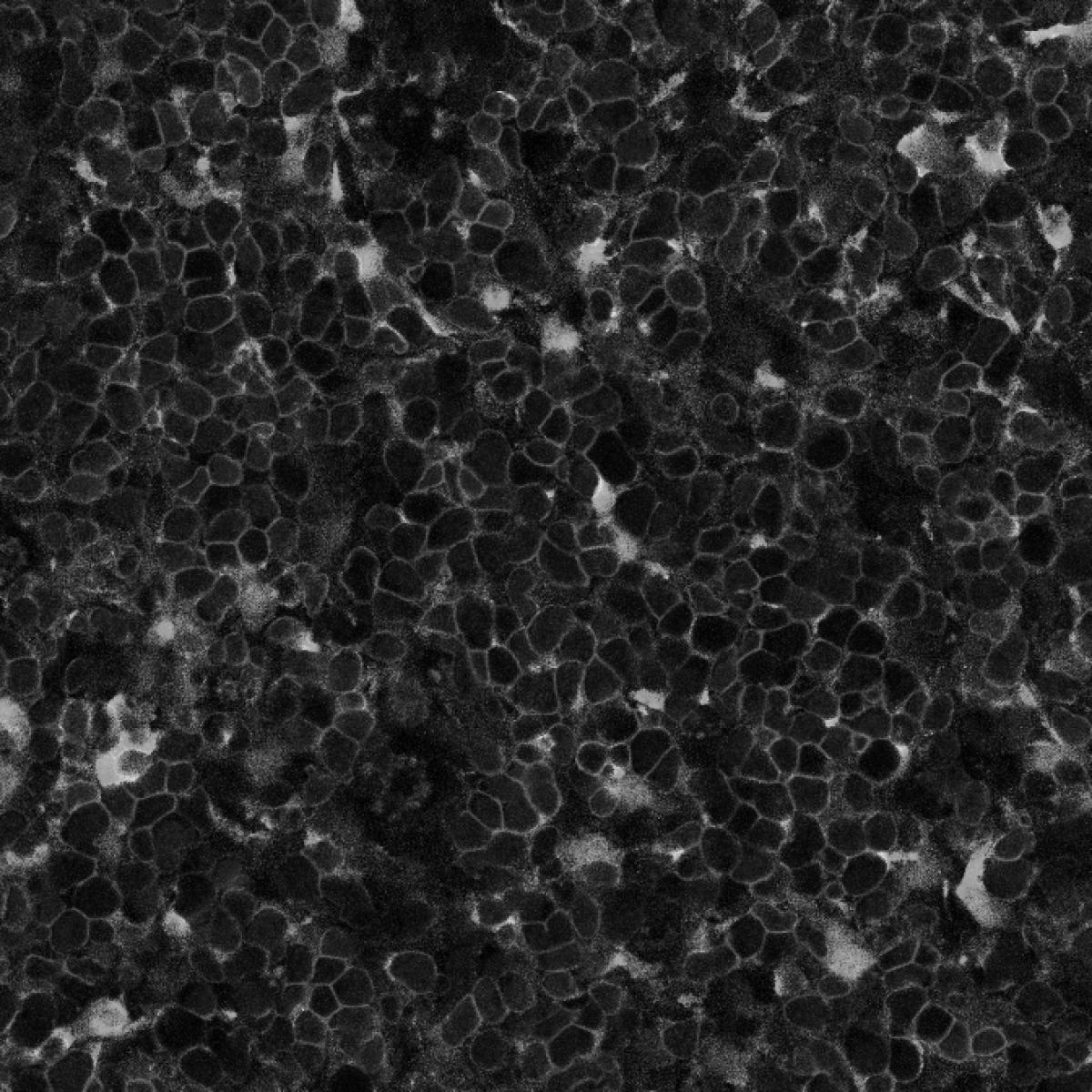
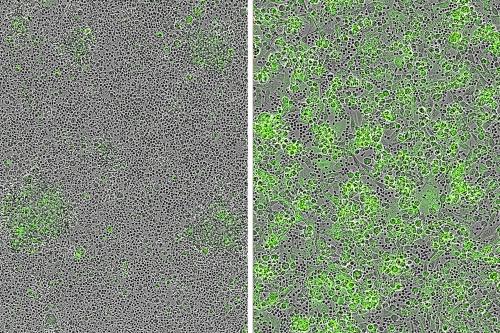
Puig-Saus combines cutting-edge genetic engineering techniques and synthetic biology tools with cancer immunology to design and clinically translate new T-cell receptor- and chimeric antigen receptor (CAR)- engineered T-cell therapies for cancer treatment. These therapies involve modifying a patient's own T cells to enhance their ability to recognize and attack cancer cells.
A key area of Puig-Saus' research involves understanding how the natural antitumor T-cell responses induced by immune checkpoint blockade therapies — a type of treatment that helps the body's immune system recognize and attack cancer cells — act in coordination to eliminate metastatic solid tumors. Puig-Saus aims to use the insights from this research to develop potent and durable T-cell therapies.
She is currently advancing an experimental CAR-T cell therapy for melanoma through IND-enabling studies, a crucial step towards opening a clinical trial.
Research Projects
- Developing and testing a new type of CAR-T cell therapy A type of immunotherapy in which a patient’s own immune cells, called T cells, are programmed to attack tumor cells. Doctors do this by applying a special cancer-recognizing receptor, referred to as a chimeric antigen receptor, or CAR, to each T cell using gene therapy. The cells are then reintroduced to the patient by infusion. CAR-T cell therapy A type of immunotherapy in which a patient’s own immune cells, called T cells, are programmed to attack tumor cells. Doctors do this by applying a special cancer-recognizing receptor, referred to as a chimeric antigen receptor, or CAR, to each T cell using gene therapy. The cells are then reintroduced to the patient by infusion. for patients with malignant and rare melanomas
- Investigating the immune system's response to melanoma in patients who do and do not benefit from anti-PD1 therapy to identify factors contributing to potent and durable immune responses against cancer
- Designing next-generation CAR- and TCR-engineered T-cell therapies for melanoma, pancreatic cancer and other types of cancer
- Exploring pharmacologic modulations that make T cell therapies more powerful and long-lasting
-
Post-doctoral Fellowship
- Immunotherapy, UCLA, 2018
Degree
- Ph.D., Biomedicine, University of Barcelona, Spain, 2013
-