UCLA study on immune cell response could lead to more effective immunotherapy
For the first time, a research team has identified and analyzed the steps by which immune cells “see” and respond to cancer cells, providing insights into reasons some treatments may be effective for certain patients but not others.
The UCLA Jonsson Comprehensive Cancer Center scientists leading the research believe their findings will lead to better, more personalized immunotherapies – even for patients whose immune systems currently do not appear to respond to treatment.
“This is an important step forward in our understanding of what the T-cell responses “see” in the tumor and how they change over time in the tumor and in circulation in the blood,” said Cristina Puig-Saus, PhD, a UCLA Jonsson Comprehensive Cancer Center researcher, adjunct assistant professor of medicine at UCLA, and the first author of a study in Nature.
“The deeper understanding of how the T-cell responses clear metastatic tumor masses will help us design better treatments and engineer T cells in multiple ways to mimic them,” she said.
The researchers adapted advanced gene-editing technology to make unprecedented observations about immune responses in patients with metastatic melanoma receiving anti-PD-1 “checkpoint inhibitor” immunotherapy. Although immune cells called T cells have the ability to detect mutations in cancer cells and eliminate them, leaving normal cells unharmed, cancer cells often evade the immune system. Checkpoint inhibitors are designed to improve the T cells’ ability to recognize and attack cancer cells.
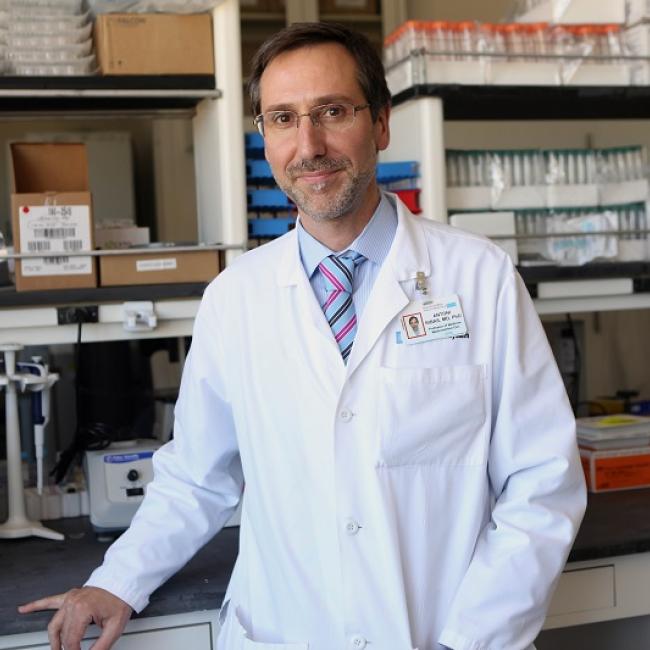
“With this work, we can know exactly what the immune system of a particular patient recognized in their cancer to differentiate it from normal cells and attack it,” said Antoni Ribas, MD, PhD, a UCLA Jonsson Comprehensive Cancer Center researcher, professor of medicine at UCLA, a co-senior author of the study.
The investigators showed that when the immunotherapy is effective, it directs a diverse repertoire of T cells against a small group of selected mutations in a tumor. These T-cell responses expand and evolve during the course of treatment, both within the tumor and in the bloodstream. Patients for whom the therapy fails also present a T-cell response against a similarly reduced number of mutations in the tumor, but those immune responses are less diverse, and they do not expand during treatment.
“This study demonstrates that patients without response to therapy still induce a tumor-reactive T-cell response,” Puig-Saus said. “These T cells could potentially be isolated and their immune receptors used to genetically modify a larger number of T cells to redirect them against the patient’s tumor. These T cells could be expanded in culture and reinfused into the patients to treat their tumors.”
In the 11 patients studied, seven had a response to PD-1 blockade; four did not. The number of mutations in the tumors ranged between 3,507 and 31. Despite this wide range, the number of mutations seen by tumor-reactive T cells ranged between 13 and one. In patients with clinical benefit from the therapy, the responses were diverse, with a range between 61 and seven different mutation-specific T cells isolated in the blood and the tumor. In contrast, in the patients lacking a response to therapy, the researchers only identified between 14 and two different T cells.
Also, in patients responding to treatment, the researchers were able to isolate tumor-reactive T cells in blood and tumors throughout treatment, but in patients without a response, the T cells were not recurrently detected. Still, the study showed that immune receptors from the T cells isolated from all patients – regardless of response or not – redirected the specificity of immune cells against the tumor, producing antitumor activity.
The work to characterize T-cell activity in patients with and without a clinical response was made possible through the creation of a new technique using sophisticated technology to isolate mutation-reactive T cells from blood and tumor samples. It builds on technology developed through a collaboration with Ribas, James Heath, PhD, president of the Institute for Systems Biology in Seattle, and David Baltimore, PhD, Nobel laureate, emeritus professor at Caltech and a member of the UCLA Jonsson Comprehensive Cancer Center.
As previously published in Nature and presented at the Society for Immunotherapy of Cancer (SITC) 2022 last November, the technology was further developed by PACT Pharma, using CRISPR gene editing to insert genes into immune cells to efficiently redirect them to recognize mutations in a patient’s own cancer cells.
“With this technique, we generated large numbers of T cells expressing the immune receptors from the mutation-reactive T cells isolated from each patient. We used these cells to characterize the reactivity of the immune receptors against the patient’s own cancer cells,” Ribas said. “The new technologies allow us to study these rare immune cells that are the mediators of immune responses to cancer.”