UCLA scientists develop novel technology that positions ‘off-the-shelf’ cancer immunotherapy for the clinic
Immunotherapies have revolutionized cancer treatment by harnessing the body’s own immune system to attack cancer cells and halt tumor growth. However, these therapies often need to be tailored to each individual patient, slowing down the treatment process and resulting in a hefty price tag that could soar well into the hundreds of thousands of dollars per patient.
To tackle these limitations, UCLA researchers have developed a new, clinically guided method to engineer more powerful immune cells called invariant natural killer T cells, or iNKT cells, that can be used for an “off-the-shelf” cancer immunotherapy in which immune cells from a single cord-blood donor can be used to treat multiple patients.
This novel technology, described in Nature Biotechnology, marks a major step toward enabling the mass production of cell therapies like CAR-T cell therapy, making these life-saving treatments more affordable and accessible to a broader range of patients.
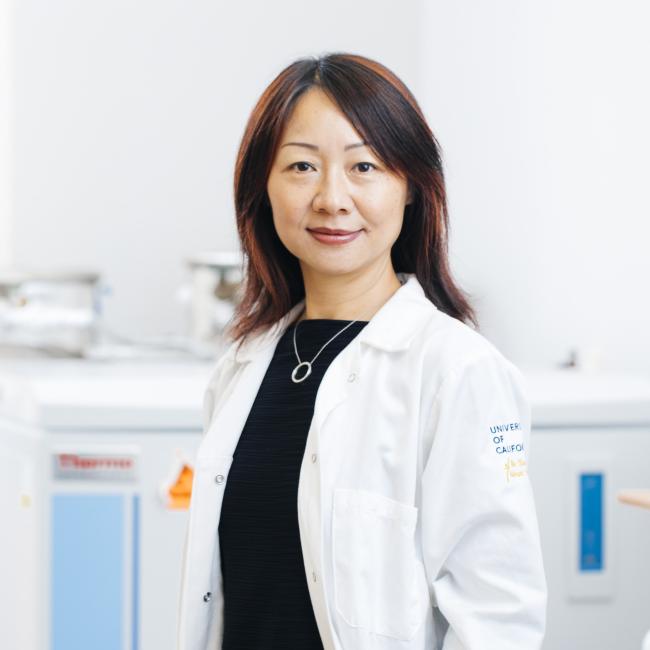
Here, the study’s senior author Lili Yang, a professor of microbiology, immunology and molecular genetics and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA and of the UCLA Health Jonsson Comprehensive Cancer Center, breaks down why this new system is poised to finally help a universal cell product advance to a clinical trial.
What are the key developments of this paper?
In 2021, our team reported a method for producing large numbers of iNKT cells using blood stem cells. That system required the use of three-dimensional thymic organoids and supportive cells, which posed both a manufacturing and regulatory challenge that prevented that method from ever reaching clinical application.
Now, we’ve developed a technology that can produce large quantities of iNKT cells from blood stem cells in a feeder-free and serum-free manner. This update to the method eliminates the previous hurdles, bringing us closer than ever to delivering an “off-the-shelf” cancer immunotherapy to patients.
How did you reach these findings?
Our team isolated the blood stem cells, which can self-replicate and produce all kinds of blood and immune cells, from 15 donor cord-blood samples representing diverse genetic backgrounds. We then genetically engineered each of those cells to develop into useful iNKT cells and estimate that one cord-blood donation can produce between 1,000-10,000 doses of a therapy — making the system really well suited to create an “off-the-shelf” immunotherapy.
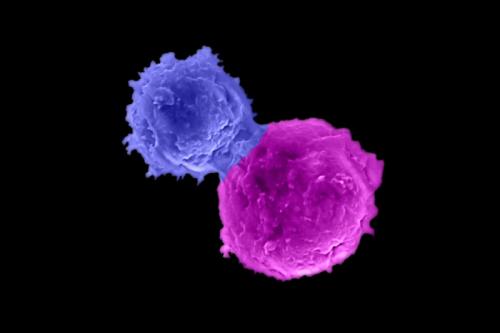
Next, our team equipped the iNKT cells with chimeric antigen receptors, or CARs, molecules that enable immune cells to recognize and kill a specific type of cancer, to target seven cancers that included both blood cancers and solid tumors. The CAR-iNKT cells showed a robust anti-tumor efficacy against all seven cancers, indicating their promising potential for treating a wide spectrum of cancers. Then in a multiple myeloma model, we demonstrated the CAR-iNKT cells’ ability to halt tumor growth without causing complications that can sometimes occur when donor cells are transplanted into a patient.
Why are iNKT cells so special?
We consider invariant natural killer T cells to be the special forces of the immune cells because they’re stronger and faster than conventional T cells and can attack tumors using multiple weapons. It’s ideal to use iNKT cells as an “off-the-self” cancer immunotherapy because they don’t carry the risk of graft-versus-host disease, a condition in which transplanted cells attack the recipient’s body and the reason most cell-based immunotherapies have to be created on a patient-specific basis.
What excites you about these developments?
No “off-the-shelf” cell therapy has ever been approved by the U.S. Food and Drug Administration, or FDA. With this new technology, not only have we shown a high output of iNKT cells, but we’ve also proven that the CAR-equipped iNKT cells don’t lose their tumor-fighting efficacy after being frozen and thawed, which is a key requirement for the widespread distribution of a universal cell product.
While CAR-T cell therapies have been a transformative treatment for certain blood cancers like leukemia and lymphoma, it has been challenging to develop a cancer immunotherapy for solid tumors. This is in part because solid tumors have an immunosuppressive tumor microenvironment, meaning the immune cell function is impaired in the environment. iNKT cells can change the tumor microenvironment by selectively and effectively depleting the most immunosuppressive cells in its surroundings — giving them the unique opportunity to attack solid tumors. We’re extremely excited that this technology has a potential broad application to target a range of blood cancers, solid tumors and other conditions such as autoimmune diseases.
What’s the biggest bottleneck in cancer immunotherapy?
The biggest bottleneck right now for immunotherapies, particularly cell therapies, is manufacturing. As of 2023, the FDA has approved six autologous CAR-T cell therapies with an average cost of around $300,000 per patient, per treatment. Using this novel technology to scale up iNKT cell production, there’s a real possibility that the price per dose of immunotherapy can drop significantly to $5,000. By definition, an “off-the-shelf” product would be readily on hand in clinical settings, so my hope is that this new system will result in a reality where all patients who need the treatment will be able to receive it immediately.
What are the next steps in the study?
Our team is advancing this multiple myeloma model project into an IND-enabling study this year, which would result in a phase 1, first-in-human clinical trial of this technology.
Since this flexible platform allows us to switch the CARs to target different cancers, our team has since adapted this same system to target ovarian cancer, one of the deadliest gynecologic cancers. This represents a big leap from targeting blood cancers to solid tumors, but we’re hopeful to bring this project to a clinical trial over the next couple of years.
Notes
Authors
The paper’s co-first authors are Yan-Ruide Li, Yang Zhou and Jiaji Yu, all from UCLA. Other UCLA authors include Yu Jeong Kim, Miao Li, Derek Lee, Kuangyi Zhou, Yuning Chen, Yichen Zhu, Yu-Chen Wang, Zhe Li, Yanqi Yu, Wenbin Guo, Xinjian Cen, Tiffany Husman, Aarushi Bajpai, Adam Kramer, Matthew Wilson, Ying Fang, Jie Huang, Shuo Li, Yonggang Zhou, Yuchong Zhang, Zoe Hahn, Enbo Zhu, Calvin Pan, Aldons J. Lusis, Jin J. Zhou, Christopher S. Seet, Donald B. Kohn, Xianghong Jasmine Zhou, Matteo Pellegrini, Benjamin R. Puliafito and Sarah M. Larson. Zachary Spencer Dunn and Pin Wang of USC and Feiyang Ma of Northwestern University contributed to the study.
Funding
This work was supported by the California Institute for Regenerative Medicine, the U.S. Department of Defense, a UCLA Broad Stem Cell Research Center Innovation Award and the Ablon Scholars Program.