UCLA scientists develop off-the-shelf immunotherapy for ovarian cancer
Key Takeaways
- UCLA researchers have developed a new type of immunotherapy called CAR-NKT cell therapy that, in patient-derived tumor samples, has been shown to be more effective at fighting ovarian cancer than conventional CAR-T cell therapy.
- Unlike current cellular immunotherapies that require patient-specific manufacturing and can cost hundreds of thousands of dollars, CAR-NKT cells can be produced off-the-shelf, lowering costs to approximately $5,000 per dose.
- The CAR-NKT platform shows promise for treating lung, brain and other solid tumors that have been challenging for CAR-T cell therapies to tackle.
Ovarian cancer is the leading cause of death among women with gynecological cancers. The current medical playbook — surgery followed by chemotherapy — initially shows promise. Tumors shrink, sometimes disappearing entirely. But in more than 80% of patients, the cancer not only comes back, but returns more aggressive and increasingly resistant to the very treatments that once seemed effective.
But now, there could be new hope. In a study published in the journal Med, UCLA researchers have detailed their development of a new type of immune cell therapy, called CAR-NKT cell therapy, that could transform ovarian cancer care by delivering superior cancer-fighting power.
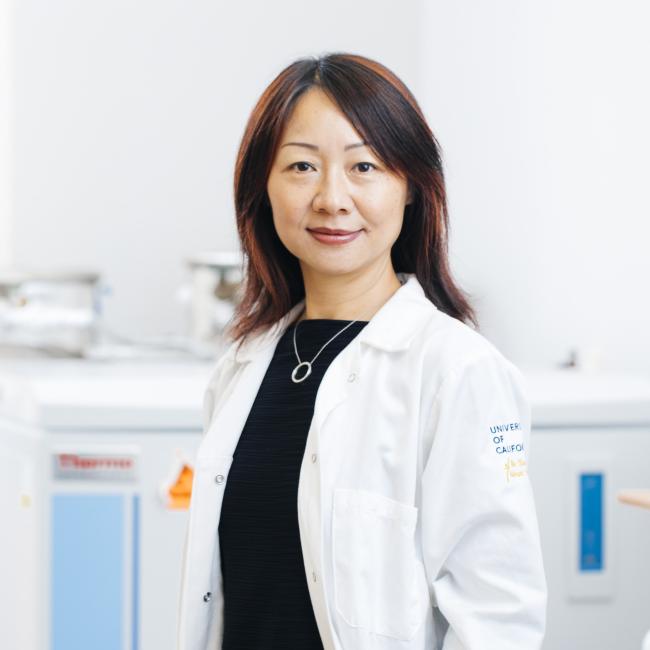
“This is the culmination of over a decade of work in my lab and represents over six years of collaboration with gynecologic oncologist Dr. Sanaz Memarzadeh,” said co-senior author Dr. Lili Yang, a professor of microbiology, immunology and molecular genetics and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA. “We’re on the verge of clinical development, and I’m genuinely optimistic that this therapy could fundamentally change how we treat ovarian cancer.”
The new therapy uses a novel platform for off-the-shelf production, making it more accessible and affordable to a broader range of patients, unlike current personalized immunotherapies that can cost hundreds of thousands of dollars.
CAR-NKT cell therapy overcomes key limitations of conventional cell therapy
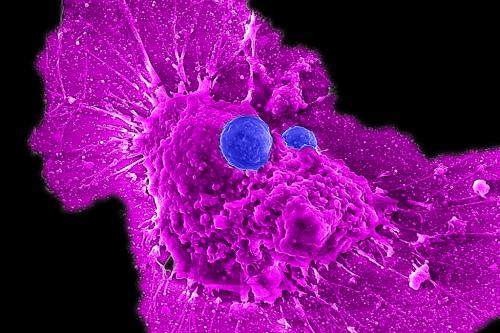
CAR-T cell therapies have revolutionized blood cancer treatment by genetically engineering patients’ immune cells into cancer-fighting weapons. However, these therapies have shown limited success against solid tumors, particularly ovarian cancer, due in part to its diverse cellular makeup and sophisticated defense systems.
To overcome these challenges, the research team’s novel CAR-NKT cell therapy harnesses a rare but powerful type of immune cell called invariant natural killer T cells, or NKT cells.
These potent tumor-fighting cells gain precision-targeting capability when equipped with a chimeric antigen receptor, or CAR.
“Cancer is like a moving target because it’s constantly changing and adapting,” said first author Yanruide (Charlie) Li, a postdoctoral scholar in the UCLA Broad Stem Cell Research Center Training Program. “The best strategy is to attack from multiple sites simultaneously.”

That’s exactly what these engineered CAR-NKT cells do. While CAR-T cells recognize only one target on cancer cells, the research team noted these CAR-NKT cells can identify dozens of molecular markers — making it extremely difficult for the cancer to escape.
This multi-target approach solves a critical problem: the cat-and-mouse game between cancer and treatment. Instead of giving tumors time to adapt and build new defenses, these CAR-NKT cells launch such a comprehensive initial attack that cancer cells can’t develop their usual resistance strategies.
Equally noteworthy, CAR-NKT cells can better penetrate the protective barrier that shields ovarian tumors from conventional CAR-T cells.
“These cells are special because they can directly kill cancer cells and also take down the immunosuppressive cells that protect the tumor,” said Yang, who’s also a member of the UCLA Health Jonsson Comprehensive Cancer Center.
Engineering the off-the-shelf treatment
The promise of CAR-NKT cell therapy extends beyond its cancer-fighting power.
Current cellular immunotherapies require collecting a patient’s immune cells, modifying them in specialized laboratories and then returning the cells to the patient — a process that can take several weeks and cost hundreds of thousands of dollars.
The CAR-NKT approach addresses these bottlenecks through a fundamentally different manufacturing method. Because NKT cells naturally work with any immune system, there’s no need for patient-specific production.
Yang’s team has developed a scalable strategy to mass-produce these cells from donated blood stem cells. A single donation could yield enough cells for thousands of treatments, lowering costs to approximately $5,000 per dose.
“Our vision is to make CAR-NKT cells available as an off-the-shelf therapy at hospitals in the U.S. and worldwide,” Yang said. “Instead of weeks-long delays for custom manufacturing, doctors could prescribe and access these cells immediately when patients need them most.”
An interdisciplinary collaboration
Early on in her clinical training, Memarzadeh witnessed a heartbreaking pattern: women with ovarian cancer would undergo treatments and experience temporary improvement, only to see their cancer return.
This experience drove her to pursue a doctorate in molecular biology and make a career-defining vow: she would tackle gynecologic cancers through both direct patient care and groundbreaking research.
That commitment has led to an ongoing partnership between Memarzadeh and Yang that shows how interdisciplinary collaboration accelerates breakthrough discoveries.
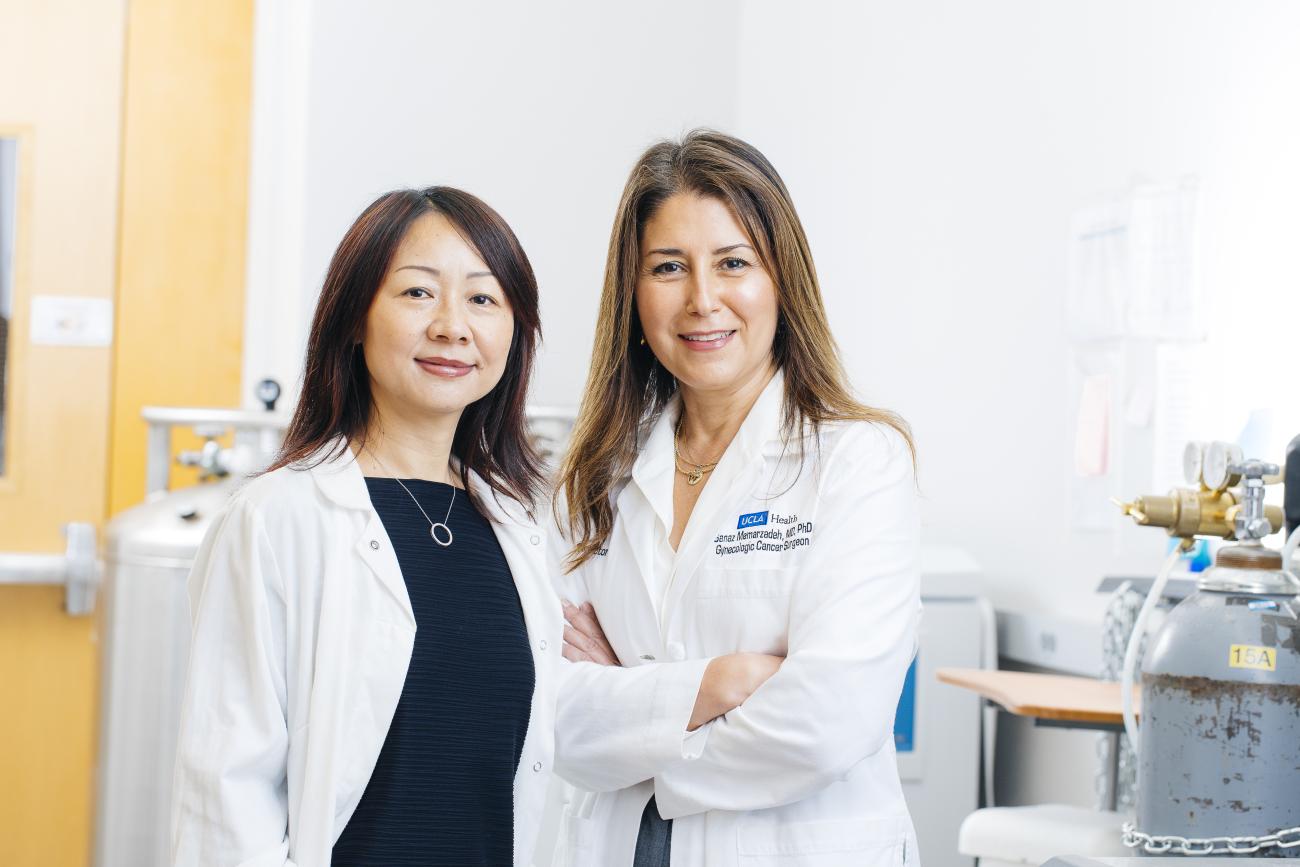
When the team tested the novel CAR-NKT therapy on 35 ovarian patient-derived tumor samples, the results were striking. The CAR-NKT cells successfully killed ovarian cancer cells in every single sample — including samples from both newly diagnosed patients and patients whose cancers had recurred after chemotherapy.
“Combating this high rate of recurrence in ovarian cancer is my career mission,” said co-senior author Memarzadeh, a professor of obstetrics and gynecology and a member of the UCLA Broad Stem Cell Research Center and the UCLA Health Jonsson Comprehensive Cancer Center. “When I see these results, I know we’re getting closer to offering patients like mine a more effective and permanent solution.”
Adopting CAR-NKT cell therapy for other types of cancer
With all preclinical studies complete, the team is preparing to submit an application to the Food and Drug Administration to begin a clinical trial.
Although ovarian cancer is their initial focus, this advancement could have much broader applications. Many solid tumors — including lung, brain and other cancers — share similar defensive mechanisms that make them difficult to treat with current immunotherapies.
“Our preclinical testing across different cancer types is showing encouraging outcomes,” Yang explained.
Additional authors include: Zhe Li, Yichen Zhu, Miao Li, Yuning Chen, Derek Lee, Christopher J. Ochoa, Tanya Singh, Gabriella DiBernardo, Wenbin Guo, Shuo Li, Yang Zhou, Yanqi Yu, Adam Kramer, Matthew Wilson, Kuangyi Zhou, Zachary Spencer Dunn, Ying Fang, Jiaji Yu, Yu Jeong Kim, Jie Huang, Xinyuan Shen, Yu-Chen Wang, Ryan Hon, Taylor Basso, Evelynn Chen, Enbo Zhu, Siyu Lin, Adam Neal, Neda A. Moatamed, Scott S. Oh, Saeed Sadeghi, Calvin Pan, Aijun Wang, Aldons J. Lusis, Xianghong Jasmine Zhou, Jin J. Zhou, Matteo Pellegrini and Pin Wang.
Notes
The research was supported by the California Institute for Regenerative Medicine, the U.S. Department of Defense, the UCLA Broad Stem Cell Research Center, the Parker Institute for Cancer Immunotherapy, the Wendy Ablon Trust, the UCLA department of microbiology, immunology and molecular genetics, the UCLA Office of the Chancellor, the UCLA Goodman-Luskin Microbiome Center, the Rose Hills Foundation and the U.S. Department of Veterans Affairs.