Discovery could lead to better recovery after stroke
UCLA researchers have identified a molecule that, after a stroke, signals brain tissue to form new connections to compensate for the damage and initiate repairs to the brain.
The finding could eventually lead to a new treatment to promote brain repair and functional recovery in people who have suffered a stroke, which is the leading cause of serious long-term disability in adults.
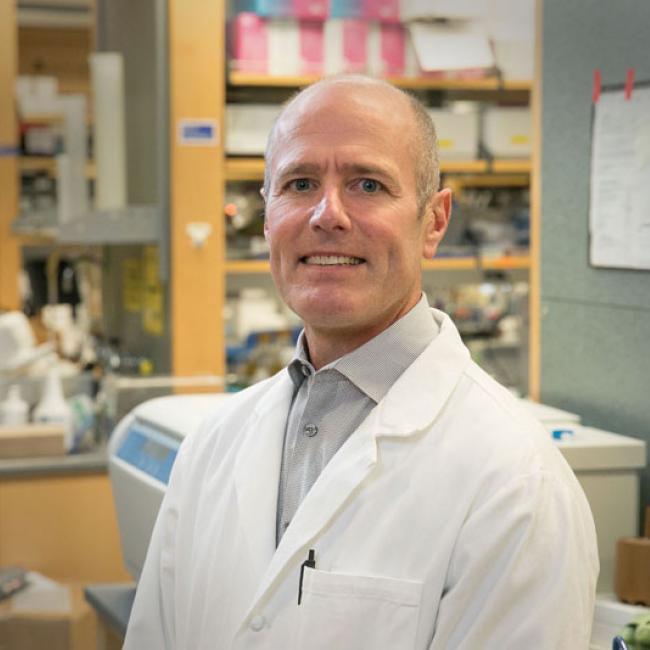
The five-year study, performed in an animal model, was the first to identify growth differentiation factor 10, or GDF10, a molecule that previously had no known role in the adult brain, said Dr. S. Thomas Carmichael, the study’s senior author, professor and vice chair for research and programs in the UCLA department of neurology and co-director of the UCLA Broad Stem Cell Research Center.
“The brain has a limited capacity for recovery after stroke,” Carmichael said. “Most stroke patients get better after their initial stroke, but few fully recover. If the signals that lead to this limited recovery after stroke can be identified and turned into a treatment, then it might be possible to enhance brain repair after stroke.”
The study, which appears Oct. 26 in the peer-reviewed journal Nature Neuroscience, also showed that GDF10 is released after a stroke in humans and in many different animals.
During a previous study, Carmichael and his team determined which molecules become more prevalent in the brain during the recovery period after a stroke, and listed all of the genes that are up- or down-regulated.
Heading into the new study, Carmichael said, researchers believed that one of the molecules on the list could be a signal telling the brain to repair itself after a stroke, and they screened for the molecules that saw the biggest increase in the brain after stroke. After finding that GDF10 was a possible signal for brain repair, the team analyzed the molecule in a petri dish.
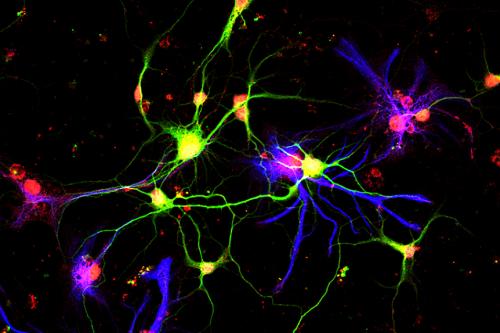
The scientists found that GDF10 promotes brain cells’ ability to form new connections, and they identified the signaling systems that control the process.
“We found that GDF10 induces new connections to form in the brain after stroke, and that this mediates the recovery of the ability to control bodily movement,” Carmichael said.
Finally, the team identified all of the molecules that are turned on or off by GDF10 in brain cells after a stroke and compared the cells’ RNA to RNA in comparable cells during brain development and normal learning, and to RNA in the brain cells of people with other diseases.
They found that GDF10 regulates a unique collection of molecules that improves recovery after stroke. The discovery indicates that brain tissue regenerating after a stroke is a unique process rather than just a reactivation of the molecules that are active in brain development.
The team also administered GDF10 to the animals that had experienced strokes and then mapped the connections in the brain that are tied to body movement. They compared those to the connections in animals who had experienced a stroke but were not given GDF10, in animals with healthy brains and with animals that had experienced a stroke and had a reduced level of GDF10.
“The results indicated that GDF10 normally is responsible for the very limited process of the formation of new connections after stroke,” Carmichael said. “Delivering more GDF10 markedly enhances the formation of new connections and does so mostly in a specific brain circuit. The formation of connections in this circuit with GDF10 administration significantly enhanced recovery of limb control after stroke.”
Going forward, Carmichael and his team hope to identify a small molecule that activates the GDF10 signaling systems and that could eventually lead to the development of a drug to enhance recovery from strokes.
Stroke kills nearly 130,000 Americans each year — one of every 20 deaths in the U.S. — according to the Centers for Disease Control. Every year, more than 795,000 people in the U.S. have a stroke, about 610,000 of them for the first time. Stroke costs the U.S. an estimated $34 billion each year, including the cost of health care, medications and missed days of work.
The study was funded by the National Institute of Neurological Disorders and Stroke at the National Institutes of Health, the American Heart Association, the Richard Merkin Foundation for Neural Regeneration at UCLA, the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation and the Edwin W. and Catherine Davis Foundation.