Brigitte Gomperts, M.D.
- Associate Director, Translational Research, UCLA Broad Stem Cell Research Center
- Professor, Pediatrics
- Professor, Pulmonary Medicine
- Co-Director, Cancer Stem Cell Biology, UCLA Health Jonsson Comprehensive Cancer Center

Brigitte Gomperts, M.D., serves as the associate director of translational research at the UCLA Broad Stem Cell Research Center. In this role, she establishes systems to facilitate the translation of basic science discoveries into therapeutic interventions and supports the progression of these therapies into clinical trials.
Gomperts is a physician-scientist who studies lung repair and regeneration to understand how these processes may go awry and lead to lung diseases. She seeks to develop new stem cell and gene therapies for diseases like idiopathic pulmonary fibrosis and cystic fibrosis.
In her clinical practice, Gomperts treats young children with cancer and blood diseases. Observing the side effects that chemotherapy, radiation and bone marrow transplant had on her patients’ lungs, Gomperts became interested in the role stem cells play in repairing lungs after injury. She has since made significant contributions to the fields of lung stem cell biology and lung repair and regeneration.
Gomperts has been at the forefront of studying the biology of idiopathic pulmonary fibrosis and the effects of environmental exposures, as well as developing gene therapeutic strategies for cystic fibrosis and new therapies for COVID-19. By studying the tissue-specific stem cells of the epithelium of the upper airways — the layer of cells that are directly in contact with everything that is breathed in — Gomperts discovered a molecule that helps maintain a balance of healthy cells in airway and lung tissue. This finding could lead to new drugs to treat or prevent lung cancer.
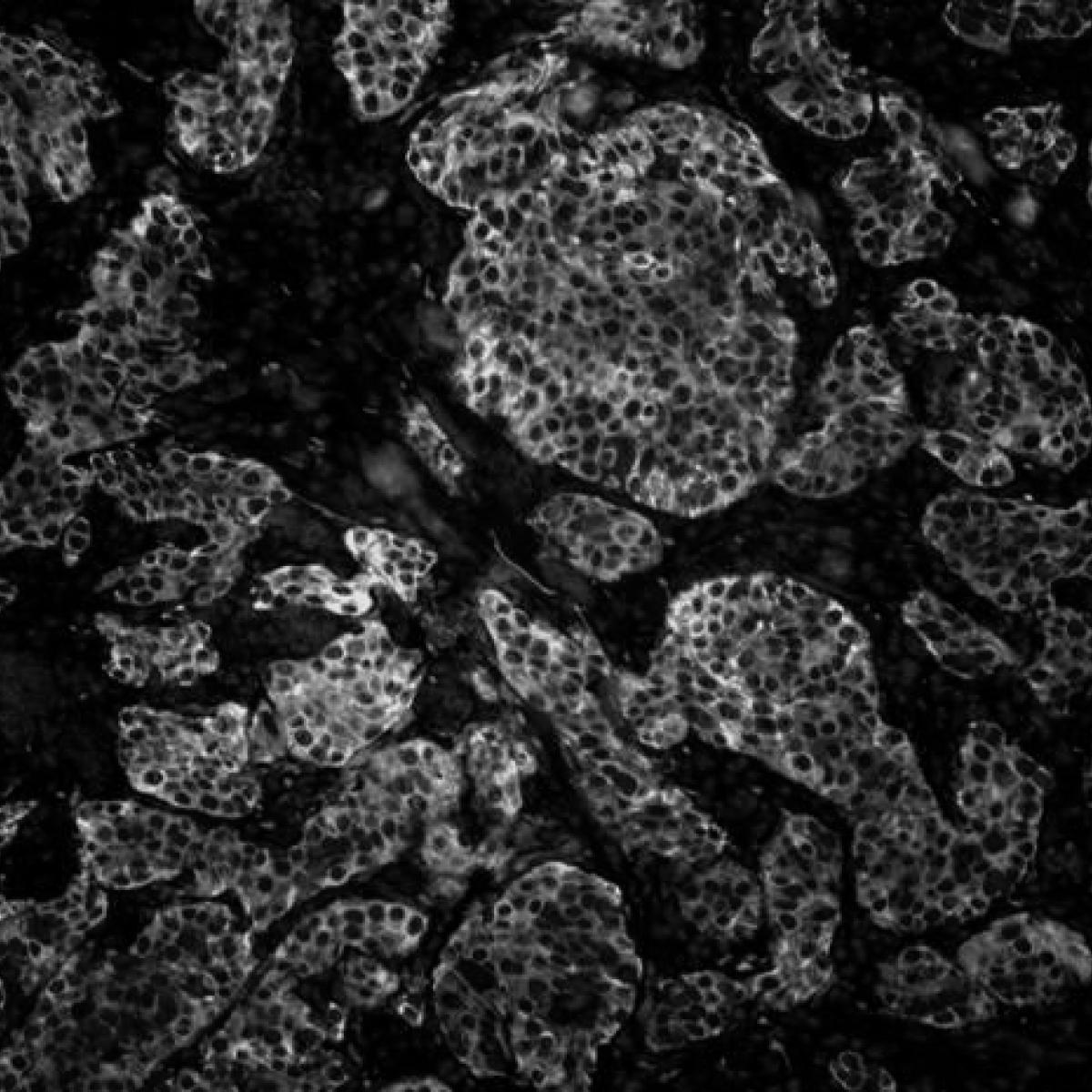
Gomperts innovated methods to generate human stem cell-derived 3D lung organoids that reflect the cell type diversity and architecture of the human lungs. These organoids are grown by coating tiny gel beads with human lung-derived stem cells and then allowing them to self-assemble into the shapes of the air sacs found in the lungs. She has used these organoids to gain critical insights into the basic biology of lung diseases and the early stages of lung cancer — and to screen for novel therapies for these conditions. Gomperts is also using these models to study how environmental exposures, which are even more relevant today because of climate change, affect the lungs. This research could influence FDA regulation of inhaled novel tobacco products and other inhaled toxins.
She has also developed a “scar in a dish” model that uses multiple types of cells derived from human stem cells to closely mimic the progressive, out-of-control scarring that can occur in human organs. This process, called fibrosis, plays a major role in many diseases and conditions, including chronic kidney disease, liver cirrhosis, idiopathic pulmonary fibrosis, scleroderma and heart failure. Gomperts is using this model to develop therapies to not only halt but reverse this process.
Research Projects
- Studying the subpopulations of cells in the airway to identify the stem and progenitor cells Descendants of stem cells that can further differentiate to produce one or more specialized cell types. They are more limited than pluripotent stem cells in that they cannot self-renew indefinitely and can only produce a limited range of specific cell types. For example, neural progenitor cells can only produce neurons. progenitor cells Descendants of stem cells that can further differentiate to produce one or more specialized cell types. They are more limited than pluripotent stem cells in that they cannot self-renew indefinitely and can only produce a limited range of specific cell types. For example, neural progenitor cells can only produce neurons. that could be targeted for a cystic fibrosis Excessive scarring within an organ due to disrupted healing. It can lead to organ dysfunction and is associated with conditions like chronic kidney disease, liver cirrhosis and heart failure. fibrosis Excessive scarring within an organ due to disrupted healing. It can lead to organ dysfunction and is associated with conditions like chronic kidney disease, liver cirrhosis and heart failure. gene therapy A technique that uses a gene or gene(s) to prevent, treat or cure a disease or disorder. Most gene therapies work by adding a healthy version of a gene to replace one that is defective or missing into the genome of particular cells. Some of these therapies use viral vectors to deliver genes into target cells. gene therapy A technique that uses a gene or gene(s) to prevent, treat or cure a disease or disorder. Most gene therapies work by adding a healthy version of a gene to replace one that is defective or missing into the genome of particular cells. Some of these therapies use viral vectors to deliver genes into target cells.
- Identifying new therapies that address the effects of cigarette smoke on SARS-CoV-2 infection using high-throughput screening of human lung models
- Developing human lung organoid 3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures. organoid 3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures. models of idiopathic pulmonary fibrosis to inform treatment development and improve understanding of the disease biology
- Studying the mechanisms that drive airway homeostasis and chemoresistance in small cell lung cancer
- Understanding the toxic effects of cigarette and vape smoke on the airway system utilizing models to mimic the unique microenvironments of the lungs
-
Medical Board Certification
- Pediatric Hematology-Oncology, American Board of Pediatrics, 2002
Fellowship
- Pediatric Hematology-Oncology, Washington University School of Medicine, 2002
Residency
- Pediatrics, Washington University School of Medicine, 1999
Internships
- Pediatrics, Washington University School of Medicine, 1996
- Internal Medicine, Johannesburg General Hospital, 1994
Degree
- M.D., University of the Witwatersrand Medical School, 1993
-