Ovarian cancer hits 'below the belt.' This doctor is raising an army to stop it
Dr. Sanaz Memarzadeh puts ovarian cancer in her sights, and she’s not giving up until she solves the mysteries of this too-often-fatal diagnosis.

The twenty-teens were rough years for Flower Miller. In 2013, one of her twin daughters was diagnosed with type 1 diabetes. Miller, then in her early 40s and the mother of three girls (her eldest daughter would also be diagnosed with diabetes two years later), was still riding the steep learning curve of understanding how to manage her child’s illness when, nearly a year after the diagnosis, she started experiencing troubling symptoms of her own. She was often bloated, and she found herself waking up more frequently at night to use the bathroom. After just a few bites of food, she felt full. Given what she was going through with her daughter, Miller chalked it up to stress.
“I was so high-stress, and so I had some symptoms that were vague,” Miller says. “I’m a woman — we just brush them off.”
When she saw her gynecologist in January 2014, everything, including her pap smear, was normal. But by April, her stomach was bloated and hard, as if she were pregnant, even though a pregnancy test indicated she was not. “That’s when I was, like, ‘Hey, this is not normal,’” she says.
Miller’s gynecologist initially suspected irritable bowel syndrome. But when she pressed on Miller’s abdomen, the doctor could feel her ovaries were swollen, and she immediately ordered a CT scan. The results showed spots throughout Miller’s abdomen. The diagnosis: ovarian cancer.
“I asked her what the outcome might be — I thought maybe she would tell me it’s treatable and we can do A and B and C — but she just took my hand and said, ‘Well, there’s hope.’ And I thought, ‘She’s telling me that I’m dying.’ I was terrified,” Miller says.
“I was so high-stress, and so I had some symptoms that were vague. I’m a woman — we just brush them off.”
— Flower Miller
The doctor referred Miller’s case to the UCLA Health tumor board, a group of oncologists and other specialists who collectively discuss and make decisions about a patient’s care. Sanaz Memarzadeh, MD (RES ’00, FEL ’03), PhD ’08, a gynecologic-oncology surgeon, was on the panel and took her as a patient. Miller knew little about ovarian cancer, only that it typically is deadly, and she spent the days before her first meeting with Dr. Memarzadeh preparing for the worst. As much as it distressed her to consider the possibility that she might die, she invited a group of moms to her home to show them how to treat her daughter’s diabetes — if she were no longer around to do it.
But Dr. Memarzadeh had a completely different vision. She laid out her plan for Miller’s treatment: surgery, chemotherapy, another surgery, additional chemotherapy and, finally, remission. “You really think I can get to remission?” Miller remembers asking. “And Dr. Memarzadeh said, ‘That’s what we do.’”
That positive attitude, and the attentive care she received at Dr. Memarzadeh’s hands, shifted Miller’s own attitude toward survival. “I just thought, OK, that’s a total game changer. It flipped,” she says.
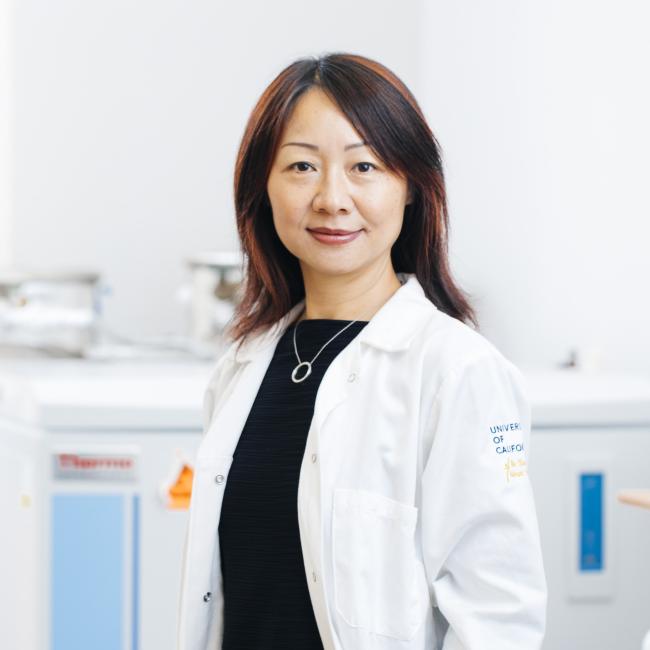
Miller, now moving toward her 11th year of remission, knows she is one of the lucky ones. The majority of women diagnosed with ovarian cancer — 80% — eventually succumb to it. More than 300,000 women worldwide are diagnosed with the disease annually, and it kills approximately 13,000 American women each year. It is patients like these who drive Dr. Memarzadeh, a physician-scientist and director of the G.O. Discovery Lab (its motto: “Engineering hope for women with cancer”) in the UCLA Broad Stem Cell Research Center, to assemble a team of world-class researchers from UCLA and beyond. Together, they are harnessing insights, tools and technologies from a multiplicity of disciplines in order to focus the most leading-edge science on this particularly deadly scourge.
“My life’s goal is to make sure that when we treat a patient with ovarian cancer, we eradicate the cancer,” Dr. Memarzadeh says. “And if a woman is facing relapse, we provide treatments that can eliminate the cancer so that it does not come back again.”
Ovarian cancer is difficult to treat for reasons that range from the subcellular to the social. Some of its unique biological features — its location in the peritoneal cavity and the microenvironment around its tumor cells — make it highly resistant to treatment. Its status as, in Dr. Memarzadeh’s words, a “below-the-belt” cancer means research on it has historically been underfunded. In fact, Dr. Memarzadeh says, ovarian cancer has one of the lowest funding-to-fatality ratios of all cancers.

This also makes it difficult for Dr. Memarzadeh to trace family histories of the disease with her patients, since people may be reluctant to discuss gynecological issues with family members. And as Miller experienced, its symptoms are vague enough that many women don’t recognize it, or they brush them off, so it often is not diagnosed until it’s at an advanced stage. All of these factors compel Dr. Memarzadeh to bring every scientific resource she can muster to the fight against it.
The most essential of these are her colleagues. “A major effort of mine has been to talk to my colleagues, who I think are brilliant, and try to get them excited to work with us on ovarian cancer,” she says. Through collaborations with researchers from different backgrounds, she is bringing a multidisciplinary and pan-cancer approach to finding new ways to treat her patients, creating a vital link between the worlds of clinical practice and research.
To foster camaraderie, she has hosted many of her scientific collaborators at her home for group dinners, providing food and drinks and then inviting them to discuss studies on ovarian cancer that she’s selected in advance. “My colleagues in science are acutely aware of the importance of clinical translation of the work, and equally are passionate about making an impact,” she adds.
Since she was a young girl growing up in Iran, Dr. Memarzadeh had an interest in science. Instead of playing with dolls, she was fascinated by the workings of nature. “I loved taking a seed and watching it grow to become a plant,” she says. “Most of the girls would play with Barbies and other toys, but I was more interested in doing experiments.”
Her mother was a nurse and her father an anesthesiologist, so it wasn’t long before she first visited a hospital. Dr. Memarzadeh’s family emigrated to the United States when she was a teenager, and she majored in neuroscience at the University of Pittsburgh, completing her studies in just three years. She jumped immediately into medical training there, where her omnivorously curious mind latched onto several specialties. At one point, she landed with a group of surgeons who were also researching immunology related to pancreatic cell clusters called islets, and she became fascinated by immunology and the practice of surgery. She was also intrigued by the scientific aspects of reproductive biology, and for a time thought she would become an infertility doctor.
But during her residency at UCLA, she spent time on the gynecologic oncology floor, where she cared for a young woman whose ovarian cancer recurred over and over, despite undergoing surgery after surgery. When Dr. Memarzadeh attended conferences seeking new research and answers, she was frustrated to see doctors recommending the same old courses of treatment that she knew were not working for her patients. “There was not enough knowledge about the disease,” she says. “I think the knowledge base, still, for gynecologic cancers is not where it should be.”
She knew that, if given the opportunity, she could make a scientific contribution. Dr. Memarzadeh entered the David Geffen School of Medicine at UCLA’s prestigious Specialty Training and Advanced Research (STAR) Program, earning a PhD in molecular biology while training under Owen Witte, MD, a renowned researcher and University Professor of microbiology, immunology and molecular genetics, who has made groundbreaking contributions to understanding of human leukemias, immune disorders and epithelial cancers, with whom she continues to collaborate.
Today, as she divides her time between the laboratory and the operating room, her work, in every sense, begins and ends with her patients. It is their health and well-being that motivates her — “My patients are my inspiration; I am struck by the bravery of the women who are facing these diagnoses,” she says — but it is also their generosity that enables her to do the research she does. As part of her clinical work, she has built a biobank of hundreds of tumor samples, as well as other biological material and health data from patients she has treated over the years.
This invaluable resource, and the passion for patient care that underpins it, has attracted collaborators from outside the school of medicine. Aaron Meyer, PhD, an associate professor of bioengineering in the UCLA Samueli School of Engineering, is among them. Dr. Meyer’s area of expertise is systems biology; he describes himself as someone who gets “very excited by understanding how the body works — the intellectual exercise of it.”
One of Dr. Meyer’s longtime interests has been antibodies, a part of the body’s immune response that, in cancer research, at least, has been overshadowed by advances in understanding and using T cells to fight cancers. But, Dr. Meyer notes, although antibodies are just proteins, they may hold important clues to harnessing the body’s immune system.
“Unlike a T cell, they’re not living — they can’t really do a whole lot on their own,” he explains. But, he continues, in their interaction with immune cells, these proteins can trigger important responses. “By recruiting cells and changing the activities of cells, they can drive things like killing cells, such as a tumor cell.”
“My patients are my inspiration. I am struck by the bravery of the women who are facing this diagnosis.”
— Dr. Sanaz Memarzadeh
One question that researchers in the 1990s had begun asking was, “Do cancer patients make antibodies against their cancer?” The answer is yes, but there was little known about it beyond that. Dr. Meyer thought that, given the advances since then in understanding the body’s immune response to cancer, he might be able to dig deeper into how antibodies fit in. But to study this, he needed access to patient samples. Colleagues at UCLA told him that Dr. Memarzadeh was very collaborative, and he knew that ovarian cancer, in particular, produced a lot of antibodies. What’s more, ovarian cancer has not been as responsive to T-cell therapies, which are more effective against other types of cancer such as leukemia and lymphoma.
“Cancer patients have these antibodies, but do they actually interact with the immune cells in the right way?” Dr. Meyer asks. In 2021, he approached Dr. Memarzadeh and explained his interests. “Sanaz has a very patient-focused perspective, so I think one of the first questions she had was, ‘OK, this is a lot of cool science, but how is this going to help my patients?’” he recalls with a laugh.
Her question prompted him to think about how he might actually apply this idea, and together they secured funding from the Mark Foundation for Cancer Research. Today, they are exploring how the antibodies produced by ovarian tumors interact with the immune system, knowledge they hope will point toward a viable therapy.
Dr. Memarzadeh had many tumor tissue samples. For her research project with Dr. Meyer, she expanded her biobank to start collecting peritoneal cavity fluid from ascites, a condition in which fluid builds up in the abdomen, and which is responsible for the bloating that is one symptom of ovarian cancer. This fluid is also rich in the antibodies they wanted to study. The scientists incubate the tumor cells with the antibody-rich fluid, wait for the antibodies to bind to the tumor cells, and then isolate those particular antibodies and tumor cells from the rest of the fluid. They then add immune-cell receptors and observe whether or not the antibodies react with those receptors to trigger an immune response.
Dr. Meyer and Dr. Memarzadeh found that these antibodies produced by tumor cells fail to interact with an important receptor known as CD16, commonly found on natural killer (NK) cells that can destroy cancer cells, and which are an important tool in cancer immunotherapy. While viruses and diseases such as COVID-19 or Epstein Barr produce antibodies that do interact with CD16, “tumor antibodies have completely lost that ability for some reason,” Dr. Meyer explains. “We’re trying to figure out how you turn that back on.”
The mechanism that makes or breaks that interaction appears to relate to a specific sugar on the bottom of the antibody, and the scientists’ next step is figuring out how to convert or modify the sugar to restore the interaction. Dr. Meyer is excited to publish this research and see if others in their field can move the science forward to a viable therapy. “There’s a lot of very creative people out there, and there’s probably going to be other labs and groups that have creative ways of developing therapies using this observation,” he says.
Another challenging aspect of treating patients with ovarian cancer is the tendency for traditional treatments, such as platinum-based chemotherapy, to lose their effectiveness. One explanation for this is that cancer cells, under pressure from therapeutic treatment, change and evolve, a quality known as “lineage plasticity.” This quality has been documented in aggressive forms of prostate and lung cancer, but when Dr. Memarzadeh saw a colleague presenting about it, she was struck by the similarity to the same pattern with high-grade serous ovarian cancer, the most common type of ovarian cancer. Working with UCLA colleagues including Thomas Graeber, PhD, professor of medical and molecular pharmacology, Dr. Memarzadeh is taking what she calls a “pan-cancer approach,” thanks to a $1.2 million grant from the U.S. Department of Veterans Affairs. “We’re taking lessons learned from other cancers and applying them to gynecologic cancers,” she says.
Another way Dr. Memarzadeh examines this resistance to treatment is by tackling it at the peptide level. Peptides are the groups of amino acids that, in combination, form proteins. They are assembled using instructions given by ribonucleic acid, or RNA, the class of molecules that essentially act as messengers between our DNA, or genetic material, and the proteins that are the building blocks of our cells, tissues, hormones and enzymes. Cancer cells, Dr. Memarzadeh notes, use these proteins to generate unique antigens, the biological signs that alert the immune system to send help. These cancer-specific proteins can emerge through a process called alternative splicing, which affects how a cell processes its RNA. Identifying these antigens, she says, would “provide a unique opportunity for targeting the cancer cells using immunotherapy approaches, while sparing the normal cells.”
Her partner in this research is Yi Xing, PhD ’06, a computational biologist and executive director of the Department of Biomedical and Health Informatics at Children’s Hospital of Philadelphia, whose work illuminates how RNA is transcribed and translated into the relevant proteins. Together, they’re using advanced computing technologies Dr. Xing and his colleagues develop in their lab to analyze a large cohort of platinum-resistant ovarian cancers, hoping to identify cancer-specific proteins by mapping out the cells’ RNA.
“Historically, and even to this day, large-scale analysis of RNA is still much more tractable than large-scale analysis of proteins,” explains Dr. Xing, who also is a professor of pathology and laboratory medicine in the University of Pennsylvania’s Perelman School of Medicine and founding director of the Center for Computational and Genomic Medicine at Children’s Hospital of Philadelphia. “By analyzing RNA, we can infer what proteins are present. It’s not a one-to-one correspondence, but the pool of RNA gives you a very good indication about the pool of proteins in the cell.”
In collaboration with hematologist-oncologist Christopher S. Seet, MD (FEL ’14), PhD ’18, and Dr. Witte, who is founding director of the UCLA Broad Stem Cell Research Center, Drs. Memarzadeh and Xing aim to engineer potent immune cells, the T cell, to target those antigens while sparing the surrounding non-cancerous tissue.
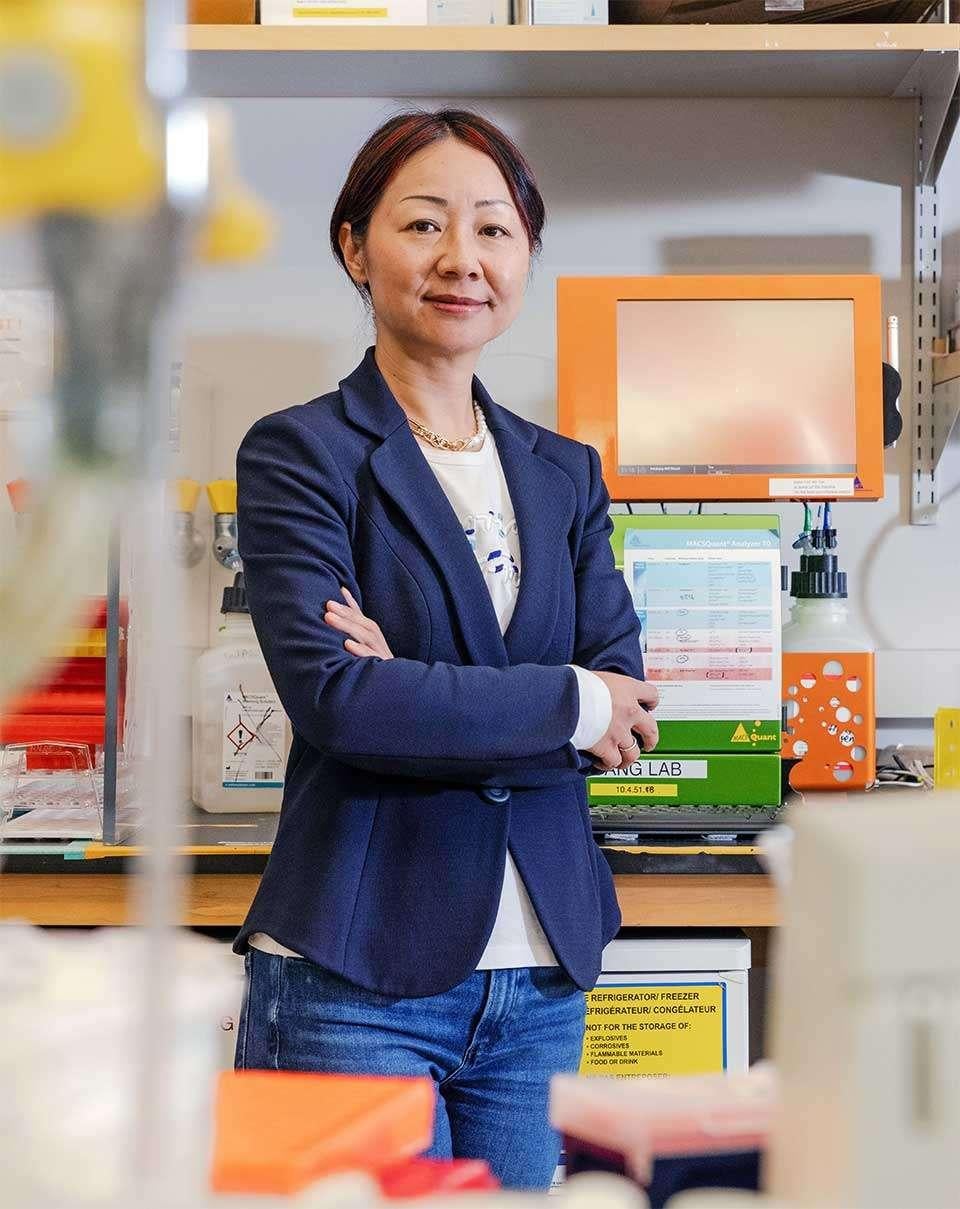
But one of the dirtiest of the many dirty tricks in ovarian cancer’s arsenal is that it’s not merely the tumor cells that fight back. Lili Yang, PhD, a professor of microbiology, immunology and molecular genetics and a member of the UCLA Jonsson Comprehensive Cancer Center, has studied many other cancers, and she says one thing that stands out to her about ovarian cancer is that its tumor cells are surrounded by a uniquely challenging microenvironment. This is in part because of its location at the base of the peritoneal cavity, which is an area of the body with a particularly high concentration of cells that inhibit an immune response. “It probably has the highest percentage of those inhibitory cells,” Dr. Yang says.
She likens them to a brick wall into which a treatment slams head-on, stopping it from working. While treatments such as immune checkpoint therapy, which allow the body’s own immune response to kick in by blocking the proteins that would otherwise inhibit it, have so far been effective in treating other cancers such as melanoma and lung cancer, not so for ovarian cancer. “Its success with ovarian cancer is minimal,” Dr. Yang says. “There’s something special about this cancer, and this could be one of the reasons.”
To address this challenge, Dr. Yang and Dr. Memarzadeh have collaborated closely, starting with a study in which they took 10 tumor samples from patients whose cancer had recurred following chemotherapy and 16 tumor samples from patients who had not yet undergone chemotherapy. By profiling how the cell populations changed before and after treatment, they could identify specific molecular targets for immunotherapies.
Dr. Yang was already working on a special type of super-charged immune cell that can fight not just the cancer cells themselves, but also the inhibitory cells that surround them. With an additional tweak, she and Dr. Memarzadeh thought it could be particularly well-suited for tackling ovarian cancer.
They eventually created what is called a CAR-equipped iNKT cell. It is bioengineered to have the features of a natural killer (NK) cell, as well as those of a T cell, the two types of cells that are the body’s main soldiers when going to war against disease and foreign pathogens. When they analyzed patient tumors, Dr. Yang says, they found that iNKT cells can target tumor cells through potent NK features, such as NK receptors, and also modulate the tumor microenvironment via T-cell receptor recognition. The T-cell component helps clear out the microenvironment of the cells that support tumor growth or prevents the immune response from working. The scientists could also identify the correct proteins to enhance these killer cells with chimeric antigen receptors, or CARs. The resulting CAR-equipped iNKT cells, referred to as CAR-iNKT cells, are capable of targeting the most highly resistant tumor cells, the ones that revert back into an almost stem-cell like state to evade attack — “the worst cells,” as Dr. Yang refers to them. This three-pronged approach has already shown promise in animal models, and Dr. Yang and Dr. Memarzadeh hope to meet with the U.S. Food and Drug Administration to explore a clinical trial by the summer of 2027, once the pre-clinical studies have concluded.
“I feel hopeful. My focus is now on what’s coming next - new clinical trials and surgeries and early detection tests and prevention.”
— Flower Miller
As she continues to move forward with her research, working hand-in-hand with collaborators at UCLA and across the country to develop new approaches and new therapies to tackle this deadly disease, Dr. Memarzadeh is committed to the fight for as long as is necessary. “I’m trying to solve ovarian cancer,” she says emphatically. “I’m not going to quit until we do.”
For Flower Miller, and Dr. Memarzadeh’s other patients, those are powerful words. “I feel hopeful,” Miller says, for herself and for other women who may face this terrible diagnosis in the future. “My focus now is on what’s coming next — new clinical trials and surgeries and early detection tests and prevention. I saw Dr. Memarzadeh the other day at a fundraising luncheon, and she had a clear message for us. ‘I’m not stopping,’ she said. And I believe her. She’s going to be the one who does it.”