Ranmal A. Samarasinghe, M.D., Ph.D.
- Assistant Professor, Neurology

Ranmal Samarasinghe, M.D., Ph.D., is a physician-scientist who treats patients with epilepsy and autism and studies the mechanisms of neural network formation and dysfunction in these conditions. He develops and utilizes stem cell-based human brain organoid models to gain insights into the causes of his patients’ diseases and to inform the creation of new treatments and cures.
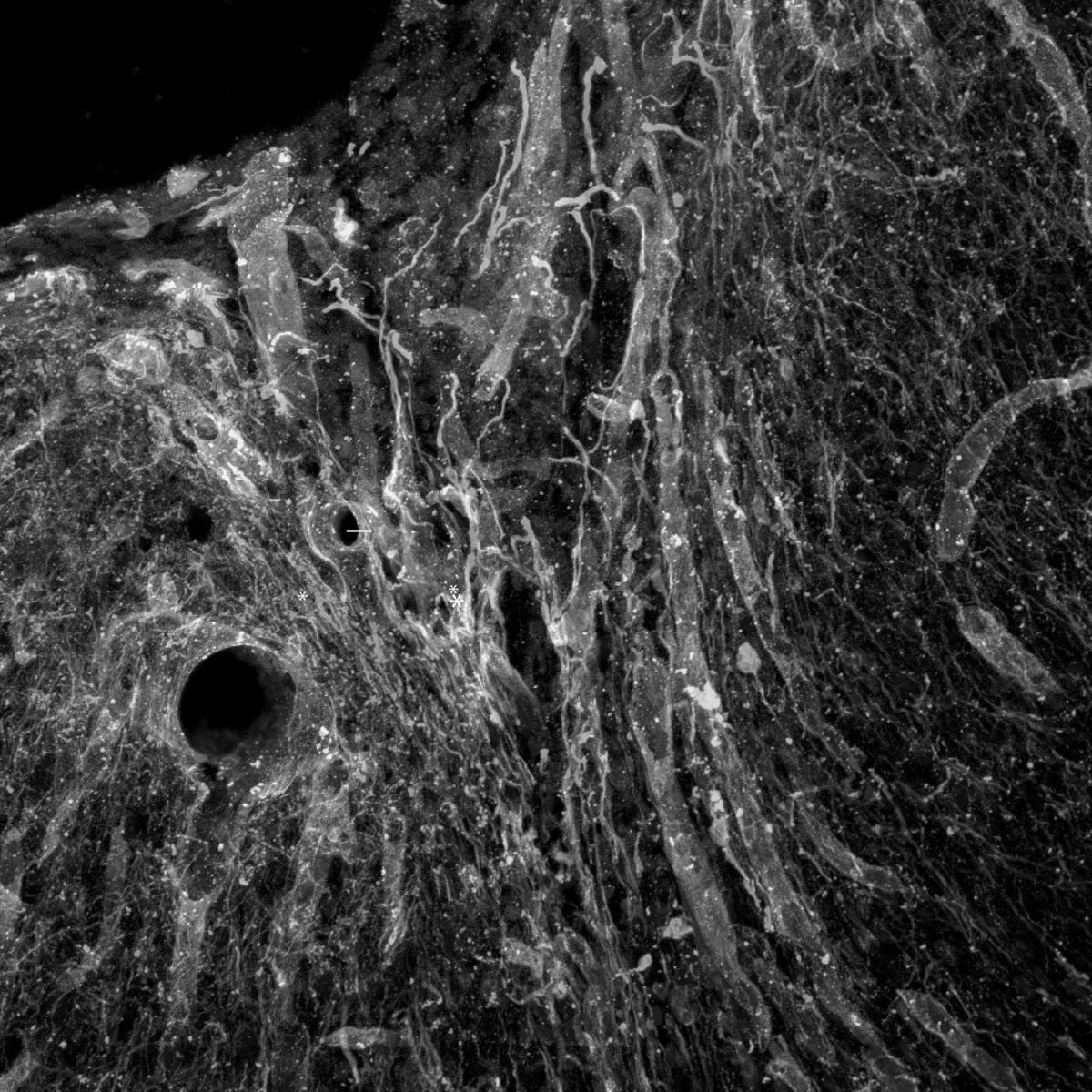
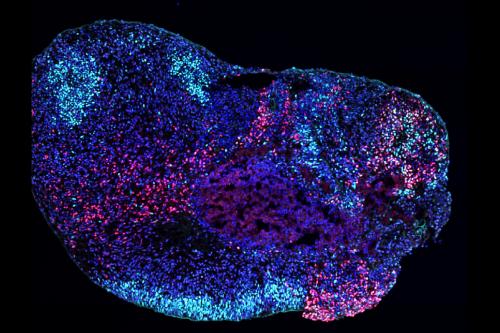
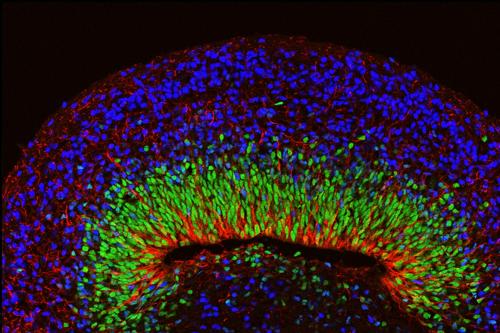
The human brain organoids Samarasinghe develops and studies are simplified 3D human brain tissue structures that are grown in the lab from human stem cells. He uses these organoids to examine the developmental processes that result in neural circuit formation; the relationship between neural circuit activity, neural oscillations and cognition; and how dysregulation of circuit formation and activity can result in neurological disease.
Because brain organoids can be generated from the stem cells of patients with epilepsy and autism, they have the potential to provide unique insights into the causes of these genetic conditions. Samarasinghe is developing and utilizing multiple methodologies including whole-organoid multiphoton-based calcium indicator imaging, voltage sensors, traditional extracellular recordings, high-throughput genomic screens and super-resolution synaptic imaging to interrogate the developmental trajectory of nascent neural networks in organoid models.
Samarasinghe is committed to refining these models and the tools required to quantify the complex physiological activities they capture, ensuring they can provide maximum value for clinical applications. This includes enabling the creation of human brain organoids generated from induced pluripotent stem cells derived from patients’ skin cells that can model the features of their disease and identify the most effective treatments for them specifically.
“New brain organoid models and the physiological data they unlock will become important tools to move us toward new treatments for epilepsy. In tandem with ongoing work in animal models, these systems will likely be complementary and paint a more complete picture of the disease process.”
- Assistant Professor, Neurology
Research Projects
- Utilizing stem cell-derived human brain organoid3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures.organoid3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures. models to determine the impact of pathogenic single gene variants associated with autism and epilepsy on neural circuit function and development
- Investigating how neural circuits develop and function in different regions of the brain
- Examining the impact of pathogenic mutations on hippocampal memory-associated circuits — which, in brain organoids that resemble the hippocampus, result in an Alzheimer’s-like dementia
-
Medical Board Certifications
- Clinical Neurophysiology, American Board of Psychiatry and Neurology, 2019
- Neurology, American Board of Psychiatry and Neurology, 2017
Residency
- Adult Neurology, David Geffen School of Medicine at UCLA, 2017
Internship
- Internal Medicine, University of Pittsburgh Medical Center, 2014
Degrees
- M.D., University of Pittsburgh School of Medicine, 2013
- Ph.D., Neuroscience, University of Pittsburgh School of Medicine, 2013
-