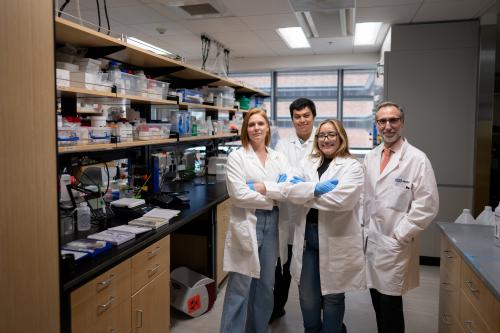
Antoni Ribas, M.D., Ph.D.
- Professor, Hematology/Oncology
- Professor, Surgery
- Professor, Molecular and Medical Pharmacology
- Director, Tumor Immunology Program, UCLA Health Jonsson Comprehensive Cancer Center
- Director, Parker Institute for Cancer Immunotherapy Center at UCLA
Antoni Ribas, M.D., Ph.D., conducts laboratory and clinical research focused on malignant melanoma, an aggressive form of skin cancer for which few effective therapies exist. He seeks to develop immunotherapy and targeted stem cell-based approaches that harness a patient’s own immune system to combat melanoma and other cancers.
For over two decades, Ribas has been at the forefront of understanding melanoma biology, investigating how the disease interacts with the immune system and translating his research into new treatments. A key focus of his research involves optimizing the treatment of melanoma through the development of tumor immunotherapy approaches and targeted therapies that are informed by a deep understanding of the biological principles governing immune cells’ antitumor activity.
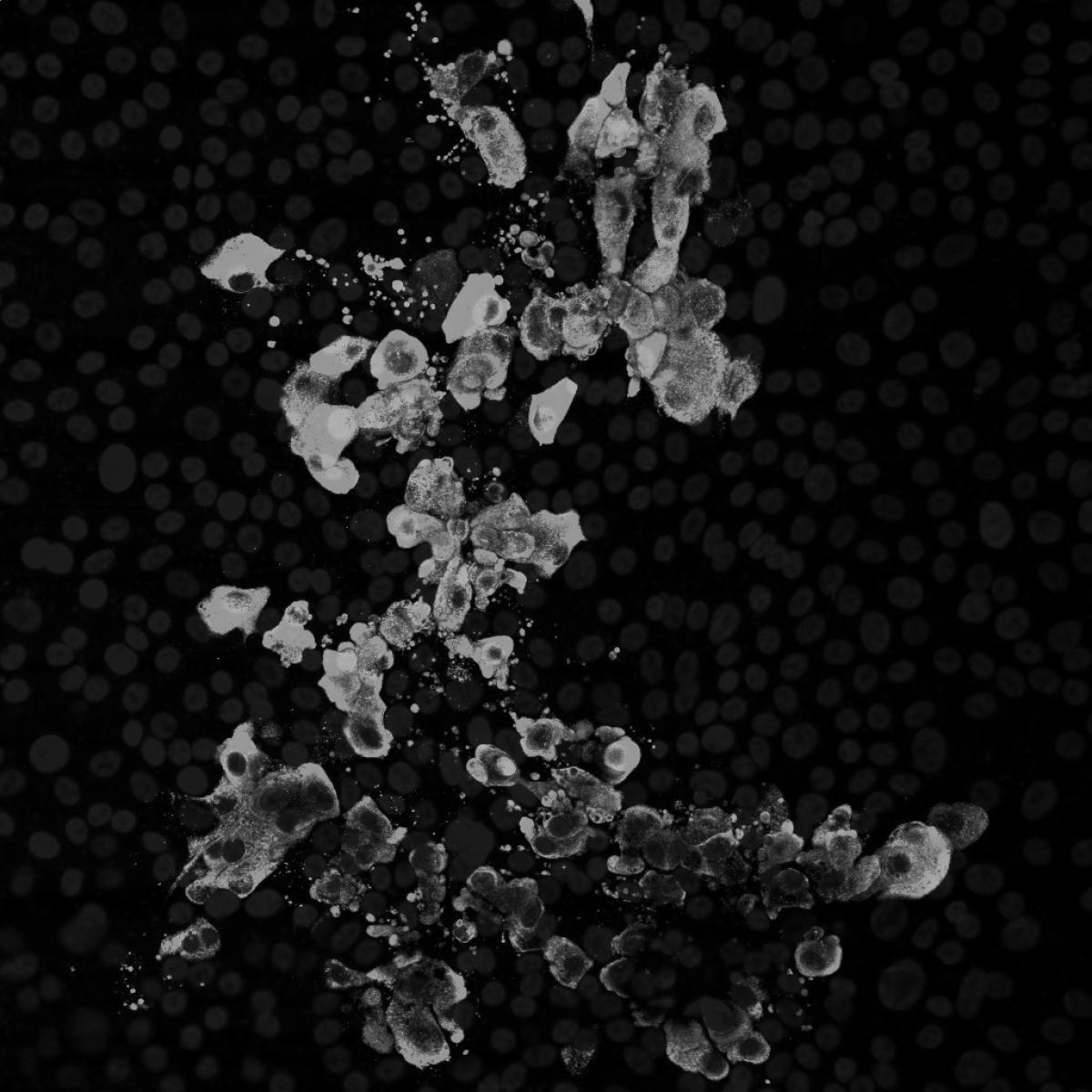
Ribas is conducting several clinical trials of cutting-edge cancer treatments, encompassing both immunotherapies and targeted stem cell-based therapies. In 2017, he launched a first-of-its-kind trial testing a dual immunotherapy approach that used both genetically modified blood stem cells and modified immune cells to treat melanomas, sarcomas and multiple myeloma. His recent work includes laboratory and clinical translational research in adoptive cell transfer therapy with T-cell receptor engineered lymphocytes, examining the antitumor activity of PD-1-blocking antibodies, testing novel targeted therapies blocking oncogenic events in melanoma and studying primary and acquired resistance to melanoma treatments.
He has been instrumental in the clinical development of several cancer therapies approved by the FDA, including the anti-CTLA-4 tremelimumab (Imjudo), two combinations of BRAF and MEK inhibitors vemurafenib (Zelboraf) and cobimetinib (Cotellic), dabrafenib (Tafinlar), trametinib (Mekinist) and the first anti-PD-1 pembrolizumab (Keytruda). Keytruda is now used in the treatment of inoperable metastatic melanoma, non-small cell lung cancers and other malignancies including Hodgkin’s lymphoma.
Ribas also utilizes molecular imaging technology such as PET scans to investigate and understand precisely how novel immunotherapies work on a molecular level. He aims to use these technologies to guide and evaluate new therapeutic strategies for melanoma.
He is a former president of the American Association for Cancer Research and an elected Fellow of the AACR Academy, the Royal Academy of Medicine of Catalonia, the American Society of Clinical Oncology and the National Academy of Medicine.
Research Projects
- Understanding how melanoma responds to or resists cancer immunotherapies
- Conducting laboratory and clinical translational research Research that focuses on “translating” discoveries into clinical practice. This research involves applying discoveries made in a lab into diagnostics, therapies and treatments that can directly benefit patients. translational research Research that focuses on “translating” discoveries into clinical practice. This research involves applying discoveries made in a lab into diagnostics, therapies and treatments that can directly benefit patients. to advance adoptive cell transfer therapies for cancer that use T-cell receptor engineered lymphocytes
- Understanding the antitumor activity of PD-1-blocking antibodies
- Testing novel targeted therapies blocking cancer-causing events in melanoma and exploring their potential to enhance immune response
- Launching a clinical trial A research study conducted with human participants to evaluate the safety and effectiveness of new medical treatments, interventions, drugs or medical devices. clinical trial A research study conducted with human participants to evaluate the safety and effectiveness of new medical treatments, interventions, drugs or medical devices. of a topical wound healing gel that could help heal chronic wounds, such as venous leg ulcers
-
Fellowships
- Hematology and Medical Oncology, David Geffen School of Medicine at UCLA, 2001
- Surgical Oncology, David Geffen School of Medicine at UCLA, 1998
Residency
- Hospital Vall d'Hebron, Spain, 1994
Internship
- Medical Oncology, Hospital Vall d'Hebron, Spain, 1991
Degrees
- Ph.D., Cancer Immunology, Autonomous University of Barcelona, Spain, 1997
- M.D., Universidad de Barcelona, Spain, 1990
-