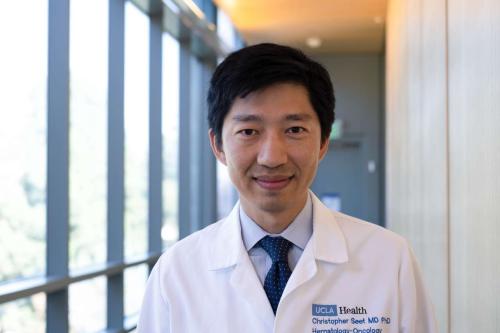
Christopher Seet, M.D., Ph.D.
- Assistant Professor, Hematology/Oncology
Christopher Seet, M.D., Ph.D., is a hematologist and oncologist specializing in blood cancers, stem cell transplantation and cellular therapies. He studies human immune cell development and function with the goal of applying his findings to develop new stem cell-based approaches to cancer immunotherapy.
Seet has made significant contributions to the study of human T cell development, including the creation of innovative techniques for modeling T cell differentiation from hematopoietic and pluripotent stem cells. As a physician-scientist, his goal is to apply these findings to address unmet medical needs, with a focus on developing therapies for hematologic malignancies.
His foundational research includes investigations on transcriptional regulation of early B cell development, B cell receptor signal transduction and leukemia stem cell biology in MLL-AF9 acute myeloid leukemia.
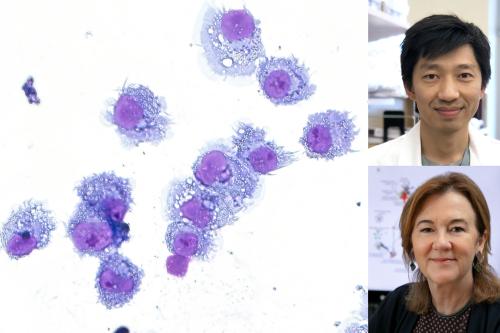
Along with center member Gay Crooks, M.D., Seet developed the artificial thymic organoid system, which enables human blood and pluripotent stem cells to become mature T cells capable of fighting infections and killing tumor cells. By mimicking the environment of the human thymus, this system also allows for accurate modeling of human T cell development. To further improve applications of this system, Seet is also investigating the differences between pluripotent stem cell-derived T cells and peripheral blood T cells and leveraging these properties toward more effective and novel immunotherapeutic applications.
Research Projects
- Generating in vitroA process, procedure or study performed in a test tube or lab dish rather than in a living organism.in vitroA process, procedure or study performed in a test tube or lab dish rather than in a living organism. tumor antigen-specific T-cell receptors for cancer immunotherapyA type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions.immunotherapyA type of treatment that uses the body's own immune system to fight cancer, infections and other diseases. This approach has revolutionized cancer care and is also being applied in experimental treatments for HIV, lupus and other conditions. using the artificial thymic organoid3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures.organoid3D tissue grown from stem cells to replicate aspects of the structure and function of an organ. By modeling how multiple types of cells interact in biologically-relevant structures, these models help researchers understand how human organs develop, age and respond to disease in more detail than 2D cultures. platform
- Enhancing the potency of T cellsWhite blood cells that naturally fight against disease-causing invaders using specialized molecules, called receptors, on their cell surface. The receptors help T cells seek out and destroy virus-infected cells or cancer cells.T cellsWhite blood cells that naturally fight against disease-causing invaders using specialized molecules, called receptors, on their cell surface. The receptors help T cells seek out and destroy virus-infected cells or cancer cells. generated from induced pluripotent stem cellsiPSCs are adult cells — typically skin or blood — that have been reprogrammed in the lab to behave like stem cells, giving them the potential to become any of the cell types found in all major tissues in the body. Because they are made from a patient's own cells, they carry that person's unique genetic code, making them a powerful tool for disease research and personalized medicineinduced pluripotent stem cellsiPSCs are adult cells — typically skin or blood — that have been reprogrammed in the lab to behave like stem cells, giving them the potential to become any of the cell types found in all major tissues in the body. Because they are made from a patient's own cells, they carry that person's unique genetic code, making them a powerful tool for disease research and personalized medicine
- Improving T cell cancer immunotherapies by characterizing novel receptor pathways in T cell-tumor cell interactions and targeting tumor immune evasion
- Identifying therapeutic targets in graft-versus-host disease following stem cell transplantation
- Developing immunotherapy approaches to treat acute myeloid leukemia
-
Medical Board Certifications
- Medical Oncology, American Board of Internal Medicine, 2019
- Hematology, American Board of Internal Medicine, 2018
Fellowship
- Hematology & Oncology, David Geffen School of Medicine at UCLA, 2014
Residency
- Internal Medicine, Loyola University, 2011
Internship
- Internal Medicine, Loyola University, 2009
Degrees
- Ph.D., Cellular and Molecular Pathology, David Geffen School of Medicine at UCLA, 2018
- M.D., University of Sydney Medical School, Australia, 2007
-