UCLA scientists receive $17.9 million in CIRM grants to advance treatments for corneal scars, HIV and vision loss
Key Takeaways
- Stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves. Stem cells Cells that have the ability to differentiate into multiple types of cells and make an unlimited number of copies of themselves. travel along a collagen network to reach damaged muscle tissue and heal it.
- In Duchenne muscular dystrophy, stiff, scarred collagen prevents stem cells from reaching their target.
- A protein called sarcospan lessens this scarring and allows stem cells to do their job more successfully, pointing toward potential new treatments for the disorder.
Researchers at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have received more than $17.9 million in grants from the California Institute for Regenerative Medicine, the state’s stem cell agency, to develop new stem cell-based treatments for corneal scarring, HIV and vision loss.
The grants awarded to Dr. Sophie Deng and Scott Kitchen are part of the CIRM Therapeutic Translational Research Program. The grant awarded to Dr. Steven Schwartz is part of the CIRM Clinical Stage Research Program.
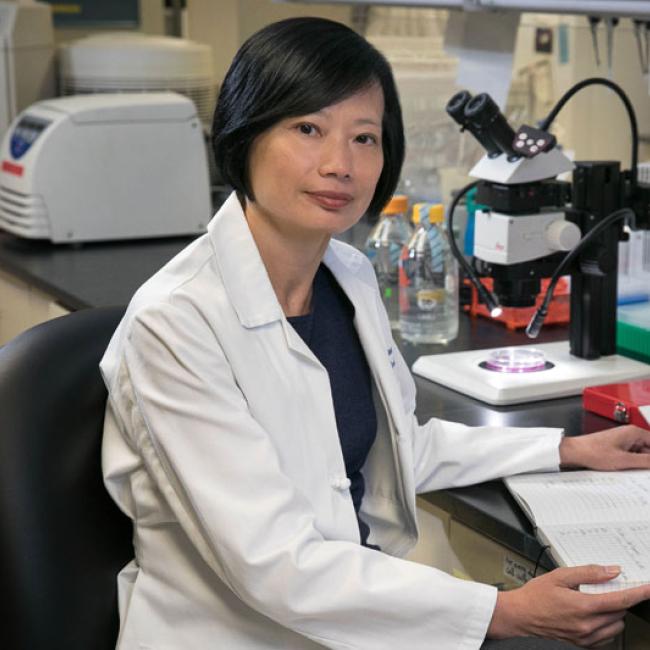
Extracellular vesicles to regenerate corneal tissue and reduce corneal scars
Sophie Deng, professor of ophthalmology
Deng’s $5.8 million award will fund the development of a new stem cell-based treatment for corneal scarring, which is the third leading cause of blindness in the world. Scars in the cornea, a consequence of injury or infection, can prevent light from passing through this outer layer of the eye and diminish vision. Today, the only way to restore vision in people with corneal scarring is with corneal transplants, which pose the risk of complications and often fail after less than a decade.
Deng’s lab has developed lines of corneal stromal stem cells— the precursors to healthy cornea cells— which have been found to reduce corneal scarring and improve vision in mice. Most recently, her team has also discovered that small spheres of molecules produced by these stem cells, called extracellular vesicles, can have the same effect as the cells themselves. These vesicles, Deng hypothesizes, could be easily applied to the eye through drops or injections and reduce the need for corneal transplants. The new funding will support Deng’s work into characterizing the extracellular vesicles, optimizing protocols to isolate them from corneal stromal stem cells, and pilot studies of their effectiveness in treating corneal scarring. Deng’s co-investigator on the project is Jie Zheng.
Immune-targeting gene therapy to treat HIV infection
Scott Kitchen, professor of medicine
$6.1 million is being awarded to Kitchen and his laboratory to develop a gene therapy that boosts the ability of people’s immune systems to fight HIV. More than three decades into the HIV pandemic, the disease can be controlled with drug-based therapies— many of which are expensive, have severe side effects and are not curative. When patients discontinue antiviral medications, their disease generally returns. Kitchen has established an approach intended to be part of a cure for HIV by modifying patients’ blood stem cells with gene therapy, which enables the production of immune cells equipped with chimeric antigen receptors, or CARs, that can recognize HIV. This not only lets the immune cells directly attack HIV-infected cells, but prevents the modified cells from becoming infected. The approach is similar to immunotherapy treatments for cancer, which harness the existing power of the human immune system to better recognize and attack diseased cells.
Extensive preclinical tests in mice have shown that Kitchen’s approach to treating HIV is safe and feasible. With the new CIRM funding, Kitchen’s laboratory will carry out all the research necessary to initiate Investigational New Drug-enabling preclinical studies. This includes further efficacy and safety testing of the gene therapy and the development of a protocol for initial human clinical trials. Kitchen’s co-investigators on the project are Anjie Zhen, Jerome Zack and Dr. Otto Yang.
Personalized stem cell therapy for blindness
Steven Schwartz, professor of ophthalmology
Schwartz will receive $6 million to advance a treatment for blinding eye conditions that uses retinal pigment epithelium, or RPE, cells created from patients’ own stem cells. The loss of the RPE, a layer of the eye that helps maintain the function of photoreceptors, is one of the final steps of many macular eye diseases— including atrophic or dry age-related macular degeneration, myopic macular degeneration and Stargardt’s macular dystrophy. There are currently no treatments for these diseases, which affect an estimated 10% of the population over age 65.
Schwartz has discovered how to harvest patients’ skin cells, reprogram those into induced pluripotent stem, or iPS, cells, and then generate patient-specific RPE cells for transplantation. With support from a previous CIRM grant, he and his colleagues tested the approach in animal models. Now, they plan to scale up manufacturing of the cells and continue research on their safety and efficacy. The new grant will support all the research necessary to file an Investigational New Drug application with the U.S. Food and Drug Administration, the first step toward launching a phase I clinical trial in two years. Schwartz’s co-investigators on the project are Zoran Galic, Dr. Donald Kohn, William Lowry, Jerome Zack, Xiaoyan Wang, Dr. Roxana Radu, Steven Nacinowitz and David Williams.
The therapeutic approaches described in this article have only been used in preclinical tests and have not been tested in humans or approved by the Food and Drug Administration as safe and effective for use in humans.