UCLA scientist receives CIRM grant to develop a cellular therapy for COVID-19 using blood stem cells
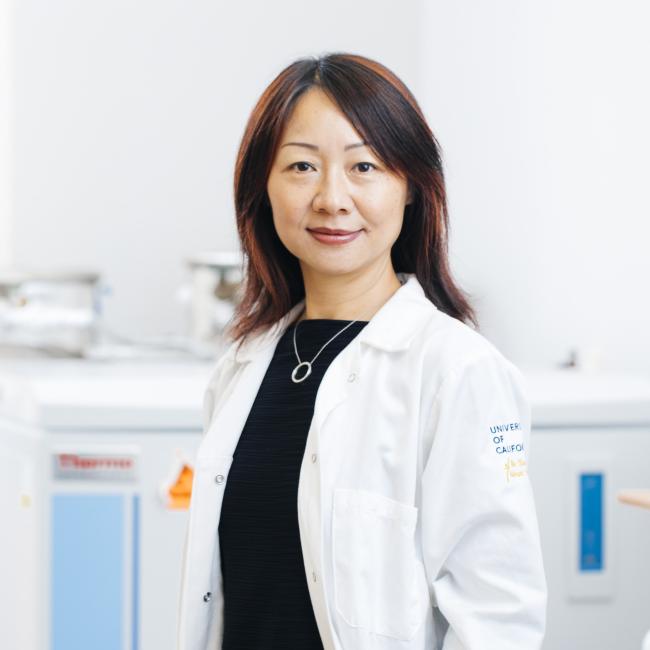
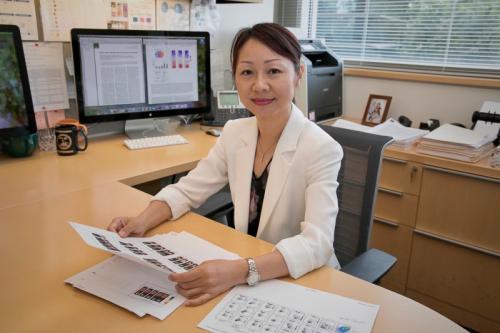
Lili Yang, a scientist at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA has received a $250,000 award from the California Institute for Regenerative Medicine, the state’s stem cell agency, to adapt a cell therapy she is developing for cancer to treat COVID-19.
The therapy will use rare and powerful immune cells called invariant natural killer T cells, or iNKT cells, grown from blood-forming stem cells, which can give rise to all blood and immune cells.
iNKT cells are a particularly promising candidate for treating COVID-19 because they have the capacity to kill virally infected cells, offer protection from reinfection and rein in the excessive inflammation caused by a hyperactive immune response to the SARS-CoV-2 virus.
This hyperactive immune response is thought to be a major cause of disease severity and death in COVID-19 patients. When the immune system overreacts to the virus, immune cells attack and inflame tissue such as the lungs, heart and kidneys, blood vessels leak and blood clots. Therapies that tamp down this excessive inflammation could greatly improve outcomes of COVID-19 patients.
“iNKT cells have an immunomodulatory function that enables them to reduce inflammation and promote tissue repair,” said Yang, an associate professor of microbiology, immunology and molecular genetics and a member of the UCLA Jonsson Comprehensive Cancer Center.
An additional benefit of iNKT cells is that they do not carry the risk of graft versus host disease, a condition in which transplanted cells attack their recipient’s body. The risk of graft versus host disease is the reason bone marrow transplants require cells from a matched donor and why many emerging therapies use a patient’s own cells that have been genetically modified or corrected. Cell therapies that do not require a matched donor or genetic modification of a patient’s own cells hold the promise to be more accessible and affordable.
Combined, these capabilities have earned iNKT cells their reputation as the special forces of the immune system. Yang has been working with these cells for years as part of other CIRM-funded projects that aim to use them to treat cancer.
“We are very close to bringing the cancer treatment to clinical trial, which means we already have the manufacturing and safety profile figured out,” Yang said. “So a big part of the work is already done. We are basically redirecting a therapy that is far along in development to treat COVID-19.”
Manufacturing has traditionally been a major impediment to the clinical application of iNKT cells, as they are extremely rare; one drop of human blood contains around 10 million total blood cells but only around 10 iNKT cells.
So, rather than using iNKT cells from the blood of healthy donors, Yang has developed a new source from which they can be abundantly derived: cord blood. This stem cell-rich blood is what remains in the placenta and attached umbilical cord after birth. After delivery, some parents opt to donate cord blood to public banks so that they can be used as stem cell transplants or in medical research.
Yang’s novel method isolates blood-forming stem cells from cord blood and then directs these cells to produce large numbers of iNKT cells. “From one single donation of cord blood, we can produce around 1,000 doses of the therapeutic level of INKT cells,” she said.
Yang envisions that these iNKT cells can be frozen and shipped to hospitals where they can then be delivered to patients via an IV injection.
Her research group is currently testing the efficacy of these stem cell-derived iNKT cells in fighting COVID-19 infection models grown using human kidney and lung cells.