
The Translational Cell Therapy Lab at UCLA: Advancing cell therapies and training future scientists
Take the elevator up to the 14th floor of the Factor Building at UCLA and you’ll find two things: striking views of the greater San Fernando Valley — marine layer permitting — and scientists covered head-to-toe in protective gear transforming scientific discoveries into new, innovative cell therapies.
Supported by the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA, the Translational Cell Therapy Lab, or TCTL, partners with investigators to advance novel therapeutic solutions for patients with often limited or nonexistent treatment options.
The TCTL specializes in cell therapies — particularly the development and safe application of induced pluripotent stem cells, or iPSCs. This approach uses a patient’s own cells to repair, replace or regenerate damaged tissues, and has the potential to transform how we treat diseases by offering potentially more personalized and curative interventions for conditions ranging from muscular dystrophies to spinal cord injuries. This class of therapies is showing increasing promise, with many advancing through the steps to widespread clinical availability. None, however, has completed a full three-phase clinical trial and secured FDA approval.
The TCTL is designed to help investigators tackle this enormous hurdle — taking a promising therapeutic candidate and turning it into a cell therapy that can be safely manufactured for patients at scale.
What the TCTL does — and why it matters
Moving from discovery to clinical application is a lengthy and complex process. It requires specialized expertise, rigorous testing and an in-depth understanding of both the science and the strict regulatory framework that governs whether a therapy is safe for patients.
“This is the space where the TCTL operates,” said director Anu Dimashkie. “If basic researchers are like the Wright brothers discovering how to fly, the TCTL is the step before Boeing — figuring out how to mass-produce planes safely and reliably.”
At its core, the TCTL helps researchers take promising therapeutic candidates and establish the protocols and processes necessary to meet FDA standards for clinical testing. While all drugs must adhere to standards set by the FDA, the regulations for cell therapies are particularly complex. These “living medicines,” require a level of precision that is significantly more rigorous than traditional pharmaceutical drugs; not only must each batch of cells be carefully cultivated, but they must also be fed, maintained and kept alive in highly sterile conditions.
This process demands expertise not just in cell biology and regulatory requirements, but also the ability to navigate the interplay between the two. At every step, TCTL scientists must ask: “How does this new result fit into our broader understanding of this cell product’s safety?” And if the answer is uncertain, “What steps must I take next to clarify it?”
Dimashkie has been instrumental in navigating the TCTL’s flagship project: helping to develop iPSC-derived retinal pigment epithelial, or RPE, cells as a potential treatment for macular degeneration, a leading cause of blindness. While scientists had learned to transform patient-derived stem cells into RPE cells in the lab, proving that these lab-grown cells were safe, reproducible and effective enough for human testing remained a significant challenge.
On May 12, after nearly a decade of work designing reliable experiments, creating robust manufacturing processes and conducting rigorous preclinical studies, her team submitted an Investigational New Drug, or IND, application — a crucial step in gaining FDA approval to begin testing the therapy in clinical trials.
Training the next generation of translational scientists
The work of the TCTL isn’t just about developing therapies; it’s about ensuring the next generation of scientists is equipped to carry this mission forward. While traditional academic or medical programs focus on research, the TCTL takes things a step further by preparing scientists for the applied, project-management-heavy world of translational medicine. At the same time, TCTL trainees and interns are taught to view every experiment through the lens of patient safety and clinical relevance.

Dimashkie emphasized that this applied, problem-solving mindset is critical to advancing patient-specific cell therapies, which represent the next frontier in medicine. These therapies will require that multitudes of scientists are trained in the hybrid set of specialized skills needed to bring this new class of “living drugs” to patients. The TCTL serves as this crucial incubator, providing hands-on experience, access to cutting-edge facilities and mentorship from experienced scientists to young researchers.
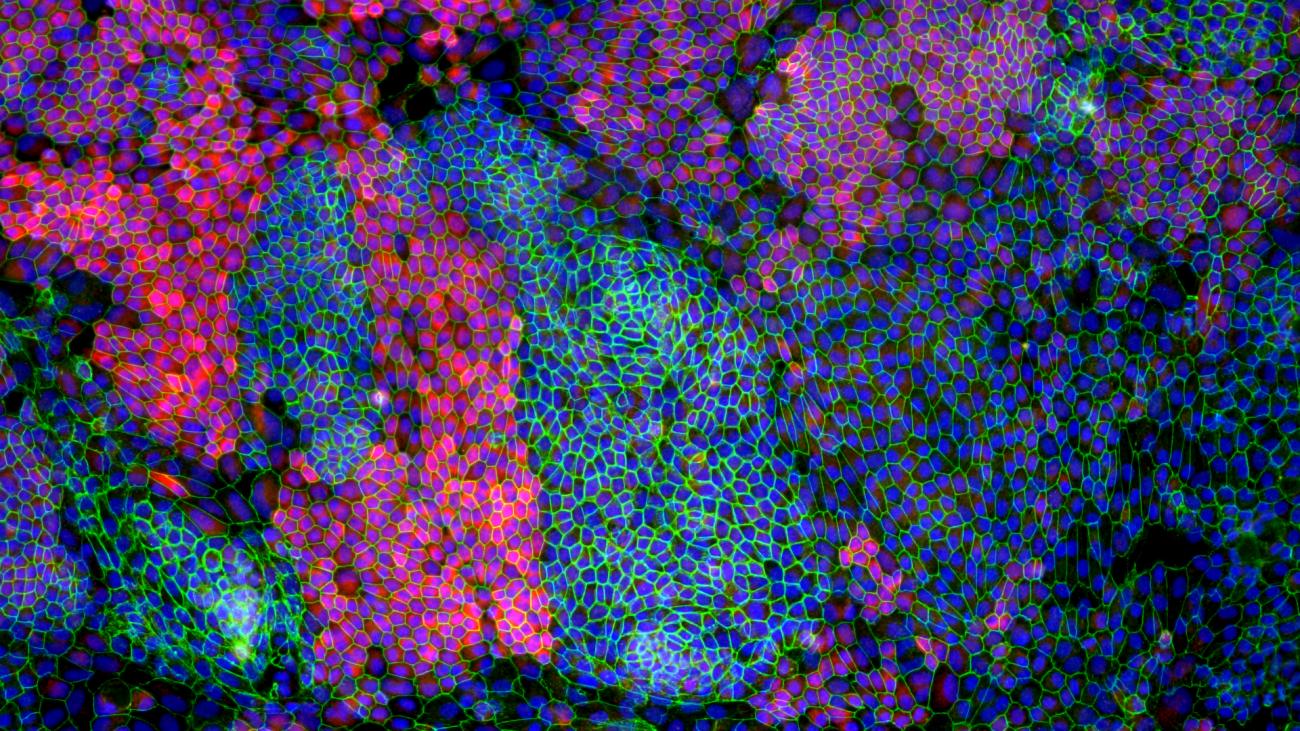
TCTL interns and trainees are introduced to experimental design, process optimization and tools for cell and tissue analysis like flow cytometry and immunohistochemistry — all while gaining an insider’s perspective on the complexities of translational research and the challenges involved in ensuring new treatments are safe, effective and reproducible.
Former TCTL trainee Talin Demirjie said that as an undergraduate studying biology at Cal State Northridge, she had limited hands-on experience with stem cells before interning at the lab.
“The TCTL opens doors for students like me who are interested in stem cells and regenerative medicine but don’t know where to gain practical experience with experimentation,” said Demirjie, who is now interning in the lab of UCLA neurobiologist Samantha Butler as part of the CSUN-UCLA Stem Cell Scientist Training Program. “It’s an incredible resource and opportunity.”
Rui Wang, another trainee, initially planned to become a practicing physician. But his time at the TCTL shifted his career aspirations, inspiring him to pursue a joint M.D./Ph.D. program. “The work at TCTL helped me appreciate the long process behind the development of new therapeutics — knowing that every single step in cell manufacturing has to meet the highest quality for the product to be safe and effective,” he said.
Meet a TCTL alumna Verna Halim
For Verna Halim, the TCTL was more than a training ground. It was the place that helped her find her footing in the scientific world.

Growing up as the child of a single mother who emigrated from Egypt, Verna spent much of her childhood in and out of hospitals due to a rare skin condition. One pivotal moment cemented her desire to pursue a career in medicine: watching her pediatric dermatologist reassure her overwhelmed mother that she was doing a great job caring for her daughter. “My mom broke down in tears,” she recalled. “The doctor had no idea how much she needed to hear that. I knew from that moment that I wanted to be that person for others.”
When Verna first joined the TCTL as a summer intern, she grappled with imposter syndrome, feeling out of place as the daughter of an immigrant family with no background in science or medicine. “But the TCTL taught me how to be uncomfortable — and how to thrive in that discomfort,” she said. “Science is about exploring the unknown, and being in uncharted waters is part of the process.”
Through hands-on experience in cell maintenance, quality control and experimental design, she gained insight into the precision and patience required in translational research. Now in her final year of medical school, Verna plans to specialize in obstetrics and gynecology while continuing to conduct research that provides a strong foundation for the care she and her fellow doctors provide. She is passionate about using her experience to drive meaningful advancements in patient care.
“If you’re not being meticulous with the way you’re practicing medicine, your patients are going to suffer,” she said. “Having people from underrepresented backgrounds in medicine means we can better understand and serve the populations we're working with. The TCTL gave me the confidence and tools to pursue this path.”
Explore more stories of impact in our special 20th anniversary report — celebrating two decades of transformative stem cell research.
