Similarities of small cell cancers to blood cancers could lead to better treatments
An interdisciplinary team of UCLA scientists has found that small cell neuroendocrine cancers from a range of tissues have a common molecular signature and share drug sensitivities with blood cancers.
The discoveries could improve the diagnoses of these aggressive cancers and lead to the development of new treatments that build upon the lessons learned from successful blood cancer therapies.
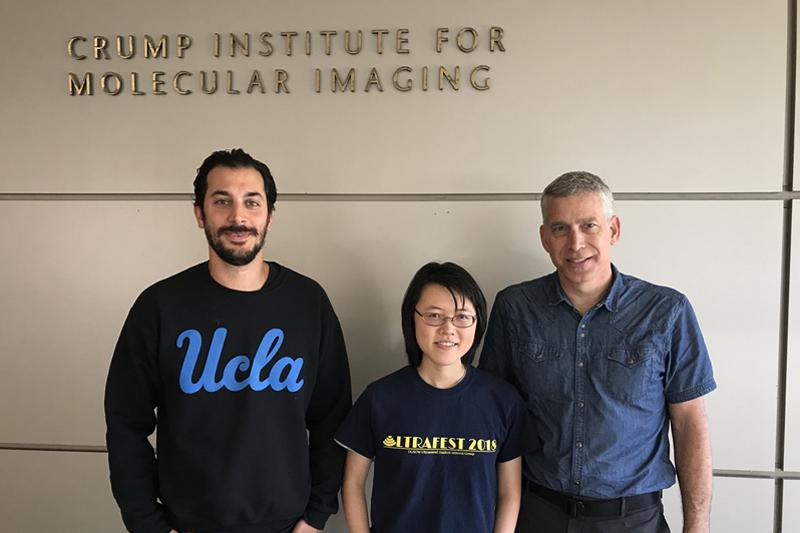
The study, led by senior authors Thomas Graeber and Dr. Owen Witte, both of the UCLA Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research and Jonsson Comprehensive Cancer Center, was published in Cancer Cell.
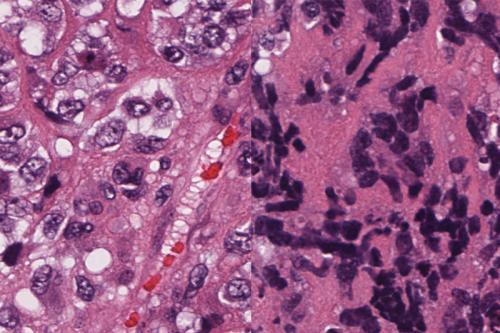
Small neuroendocrine cell cancers — also known as small cell cancers — are a deadly cancer subtype, defined by their characteristics under the microscope. They are fast-growing, treatment-resistant and can appear in a range of epithelial tissues. They are most commonly found in the lungs, with rare cases occurring in the prostate, bladder, breast and skin. Small cell cancers may become increasingly common as non-small cell cancers can transform into this highly aggressive type to resist treatment.
“Transformation to the small cell type has become an ‘escape route’ that cancers use to evade the effects of targeted therapies,” said Graeber, director of the UCLA Metabolomics Center and professor of molecular and medical pharmacology. “Our group is looking for commonalities that can be targeted by drugs to treat these cancers and prevent less aggressive cancers from transforming into this type.”
Previous research from this group found that small cell cancers of the prostate and lung have shared molecular mechanisms. For the current study, the team took a broader view by analyzing genetic and molecular data from small cell cancers originating in a wide range of tissues.
“Our research is guided by insights from the clinic, and pathologists — the doctors who closely examine tumor cells to diagnose disease — tend to describe the features of small cell cancers very similarly,” said Witte, founding director of the UCLA Broad Stem Cell Research Center and professor of microbiology, immunology and molecular genetics. “We figured if these cancers have common physical features, they likely have molecular similarities as well.”
Pursuing this hypothesis, co-first authors Nikolas Balanis and Katherine Sheu used computational methods to analyze a publicly available dataset containing genetic and molecular profiles of more than 10,000 patient tumor samples spanning more than 35 small cell and non-small cell cancer types. The algorithm they used, called principal component analysis, finds the strongest trends within large volumes of data.
Their analysis found a molecular signature that is shared across small cell cancers and cancers in the process of evolving into the small cell type, regardless of the tissue’s origin.
To validate these findings, co-author Dr. Jiaoti Huang, a former UCLA professor of pathology and urology, examined 28 tumors with the molecular signature. Huang, who now holds a chair of pathology at Duke University, determined that 26 tumors (or 93%) had detectable small cell features.
“Because these data contained patient outcomes, we were able to see that patients whose tumors bore this molecular signature had worse survival rates than people whose tumors did not have this signature,” said Balanis, a postdoctoral researcher in Graeber’s lab. “So our hope is that one day, people with cancer could have their tumors screened for this signature early on to identify when more aggressive treatment is needed.”
Even if small cell cancers can be detected sooner, there are currently no effective treatments. The team hopes its findings can help by making it easier to study small cell cancers and test potential therapies.
“Our findings suggest that things learned in small cell cancers of one tissue could apply to other tissue types,” said Sheu, a graduate student in UCLA and Caltech’s Medical Scientist Training Program. “It doesn’t have to be that you get all of your data from one cancer subcategory — you could integrate data from across tissues and advance therapies that way.”
Seeking a drug that would treat small cell cancers across tissues, the group next analyzed a drug screen database showing the efficacy of 255 currently available and experimental drugs on a wide range of cancers. They again used the principal component analysis algorithm to identify drug candidates that were effective in treating small cell cancers from multiple tissue types.
This revealed a remarkable trend: Several drug candidates that were effective against small cell cancers had the same positive results on blood cancers.
“At first, we thought there might be something wrong,” Balanis said. “But the blood connection kept showing up at every level of the molecular drug screen data.”
Tests of additional data confirmed that while blood cancers do not completely share the molecular signature the group identified, they have enough in common with small cell cancers to be sensitive to some of the same drugs. The group hopes that lessons learned in treating blood cancers could inform the development of new therapies for small cell cancers.
“I remember telling Katherine and Niko to leave blood cancers out of their initial analysis because they’re so different and may only complicate things,” Graeber said. “I’m glad they didn’t fully listen to me. Our ability to treat blood cancers is far better than our ability to treat small cell cancers, so this reveals a possible new therapeutic avenue for an incurable group of cancers that is definitely worth pursuing.”
All of the study’s drug data are from preclinical tests conducted on tumor cells in a lab dish. Additional testing will be needed to determine which, if any, of the drug candidates identified will be safe and effective in treating small cell cancers in humans.
The research was supported by the National Institutes of Health, the UCLA Specialized Program of Research Excellence in Prostate Cancer, the W.M. Keck Foundation, the UCLA Broad Stem Cell Research Center, including the Hal Gaba Director’s Fund for Cancer Stem Cell Research, the UC Tobacco-Related Disease Research Program, the UCLA Medical Scientist Training Program, the Systems and Integrative Biology Training Grant at UCLA, the Prostate Cancer Foundation and the NIH National Center for Advancing Translational Science UCLA Clinical and Translational Science Institute.

